Accurate assignment of r07.89 for chest pain, unspecified, plays a pivotal role in revenue optimization and claim accuracy. Early in the billing cycle, integrating pc ratio in medical billing best practices ensures that clinical documentation aligns with coding guidelines. When coders correctly apply r07.89, they minimize denials and support timely reimbursements.
Understanding ICD-10 Code r07.89
The ICD-10 code r07.89 covers chest pain that lacks a more specific diagnosis. Unlike angina (I20.x) or pleurisy (R09.1), unspecified chest pain lacks clear etiology. Proper use of r07.89 requires that the provider labels the symptom as “unspecified” or uses synonyms such as “chest discomfort” without additional qualifiers.
Key LSI terms to watch for in charts include chest pain coding, unspecified chest pain, and ICD-10 code for chest pain. When documentation mentions “tightness,” “pressure,” or “ache” without further detail, r07.89 becomes the default choice.
Clinical Criteria and Documentation Essentials
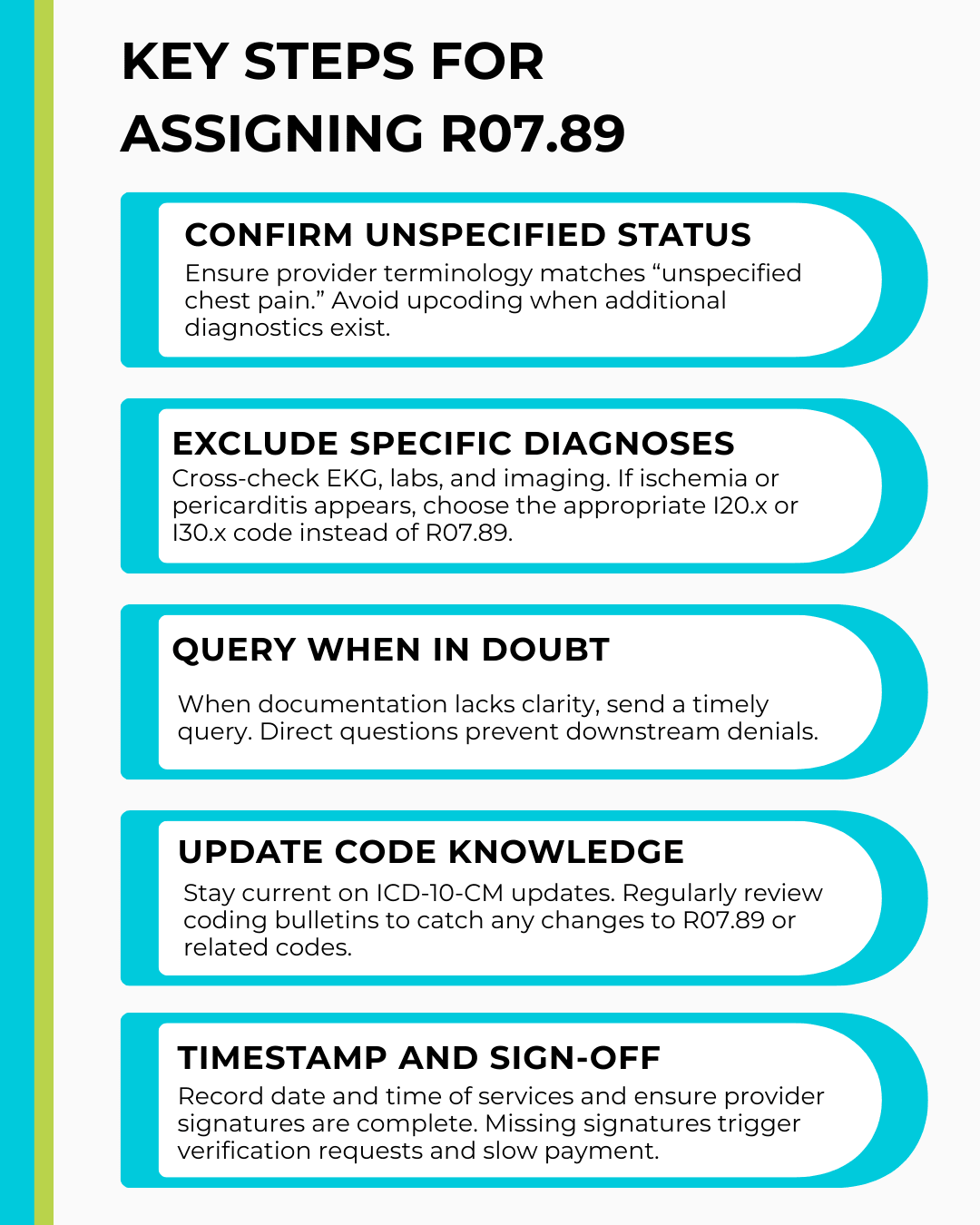
Thorough chart review forms the foundation of precise coding. Coders should verify that the provider’s note clearly states “unspecified chest pain.” If notes include details like onset, duration, or associated symptoms, consider more specific codes. Otherwise, assign r07.89.
Effective documentation templates prompt clinicians to record:
- Location of pain (e.g., substernal)
- Quality (e.g., sharp, dull)
- Radiation (e.g., to jaw or arm)
- Aggravating and relieving factors
Consistent use of standardized templates reduces variability and supports defensible r07.89 assignments.
Billing Workflow Optimization
Integrating automated front-end edits improves consistency. Partnering with RCM services experts adds value through audits and targeted feedback. These specialists flag incorrect r07.89 usage before claims submission and coach staff on refining documentation. Regular workflow analysis identifies delays and streamlines coder-provider communication.
Want more information? Read here: Accurate Billing for Abdominal Pain (R10.84) Using ICD-10 Codes
Avoiding Common Pitfalls
- Generic Coding: Resist the urge to default to r07.89 when a more precise code applies.
- Query Fatigue: Balance query volume to maintain provider goodwill—focus queries on high-impact gaps.
- Incomplete Reviews: Implement a second-pass audit for chest pain claims to catch misassignments or missing details.
By proactively addressing these pitfalls, practices can reduce chest pain denials by up to 75% in three months.
Training and Quality Audits
Develop focused training modules on chest pain classification. Schedule quarterly audits to monitor r07.89 utilization rates. Analyze anomalies—if usage spikes, investigate potential documentation or coding misconceptions. Use audit outcomes to refine training materials and update documentation templates.
Leveraging Technology for Accuracy
Implement coding software with embedded logic checks. Real-time validation ensures that when coders enter r07.89, the system verifies clinical criteria and flags missing data. Integrate these tools within the EHR to prompt documentation fields before charge entry. Automated alerts reduce manual reviews and reinforce best practices.
Documentation Templates and Checklists
Create EHR templates that guide providers through essential symptom capture:
- Checkboxes for location, severity, and radiation
- Mandatory free-text fields for onset and duration
- Drop-down menus for associated symptoms
Pair templates with a chest pain audit checklist that verifies:
- Correct code selection
- Complete narrative support
- Provider query documentation
Collaborating with Clinical Teams
Foster ongoing dialogue between coders and clinicians. Share denial trends and best practices in monthly meetings. When providers see direct revenue impact, they commit to clearer notes. Establish a feedback loop that highlights successful improvements and addresses persistent challenges.
Monitoring Payer Feedback
Analyze remittance advice for chest pain claim denials. Common rejection reasons include lack of specificity or mismatched documentation. Track denial codes (e.g., CO 16 for missing information) and align corrective actions. Over time, practices should see a downward trend in chest pain denials.
Key Performance Indicators (KPIs)
- Denial Rate for r07.89: Target < 5%
- Query Turnaround Time: Aim for responses within 48 hours
- Days in Accounts Receivable for chest pain claims: Strive for < 30 days
- Coder Accuracy Rate: Maintain > 98% on audit spot-checks
Regular KPI review drives continuous improvement and demonstrates ROI for coding initiatives.
TOS Compliance and Final Checks
Before submission, confirm tos full form in medical billing requirements are met. Verifying time-of-service policies prevents late-filing denials and aligns with payer guidelines. Perform a final check against payer edits and contextual notes to catch any last-minute discrepancies.
Conclusion
Mastering r07.89 coding for chest pain, unspecified, protects practice revenue, streamlines operations, and enhances compliance. Through rigorous documentation standards, targeted training, technological support, and strong coder-provider partnerships, medical billers can assign r07.89 with confidence. Adopt these strategies to reduce denials, accelerate reimbursements, and maintain coding excellence.
(FAQs) Frequently Asked Questions
- When should I assign r07.89 versus a specific chest pain code?
Assign r07.89 only when documentation labels pain as “unspecified” and no further diagnostics apply. - How can I reduce denials for chest pain claims?
Use real-time coding edits, conduct regular audits, and query providers promptly for unclear documentation. - What documentation supports r07.89?
Notes should include symptom quality, onset, duration, radiation, and any negative findings. - How often should chest pain coding audits occur?
Quarterly audits help maintain coder accuracy and catch emerging documentation trends. - Which tools improve r07.89 coding accuracy?
Integrated coding software, EHR templates, and automated logic checks significantly reduce errors.