Accuracy is essential in medical billing and coding, not only for compliance but also for ensuring proper reimbursement. One modifier that often confuses is modifier 53, which is used when a procedure is terminated due to extenuating circumstances after it has begun.
Whether you’re part of a large hospital or working with a medical billing company, a vital part of your revenue integrity strategy. This guide explains when and how to apply this modifier correctly, complete with examples, documentation tips, infographics, and FAQs.
What Is Modifier 53?
Is appended to a CPT code when a provider begins a procedure but must discontinue it due to:
- Patient risk or instability
- Complications during surgery or diagnostics
- Equipment failure mid-procedure
- Unexpected anatomical findings
Importantly, modifier 53 only applies when a procedure has started but is not completed for reasons beyond the physician’s control, prioritizing patient safety.
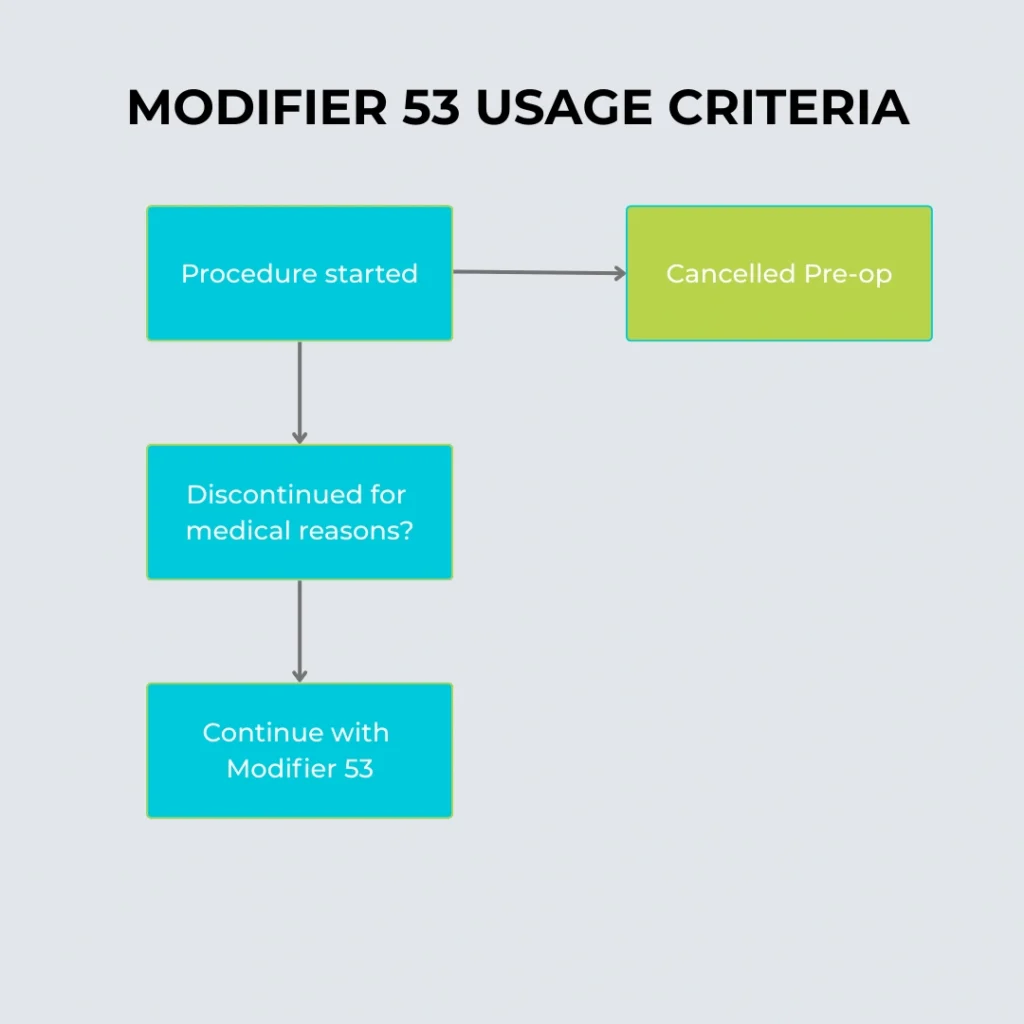
When to Use Modifier 53
Depends on both the type of procedure and the reason for its discontinuation. Here’s a breakdown:
Valid Uses:
- Colonoscopy started but was stopped due to bowel perforation
- Diagnostic laparoscopy halted due to unexpected internal bleeding
- Endoscopy was terminated because the patient experienced respiratory distress
Invalid Uses:
- Cancelled procedures before the patient is prepped
- Stopped services due to provider error or preference
- Cosmetic procedures with patient indecision midway
Partnering with professionals experienced in revenue cycle management healthcare helps ensure these distinctions are properly coded and reimbursed.
Usage Criteria
Documentation Requirements
Using modifier 53 without sufficient documentation almost guarantees claim denials. Here’s what’s needed:
- Operative or procedure note stating why the service was discontinued
- Description of the patient’s condition during the attempt
- Timeline indicating procedure initiation and termination
- Any medical complications encountered
Documentation should explain that the procedure began with the intent to complete but had to be discontinued to protect the patient.
Example Case Study
CPT Code 45378 – Colonoscopy, Diagnostic
Dr. Smith begins a routine diagnostic colonoscopy but encounters active rectal bleeding that makes it unsafe to proceed. The procedure is halted after 15 minutes.
- Bill as 45378-53
- Document: Start time, reason for termination, condition of the patient
- Outcome: Partial reimbursement with justification
This example illustrates how ensures you’re fairly reimbursed for work already performed—even if the procedure isn’t finished.
Learn More About: CPT Codes for Mental Health Professionals
Modifier 53 vs. Modifier 52
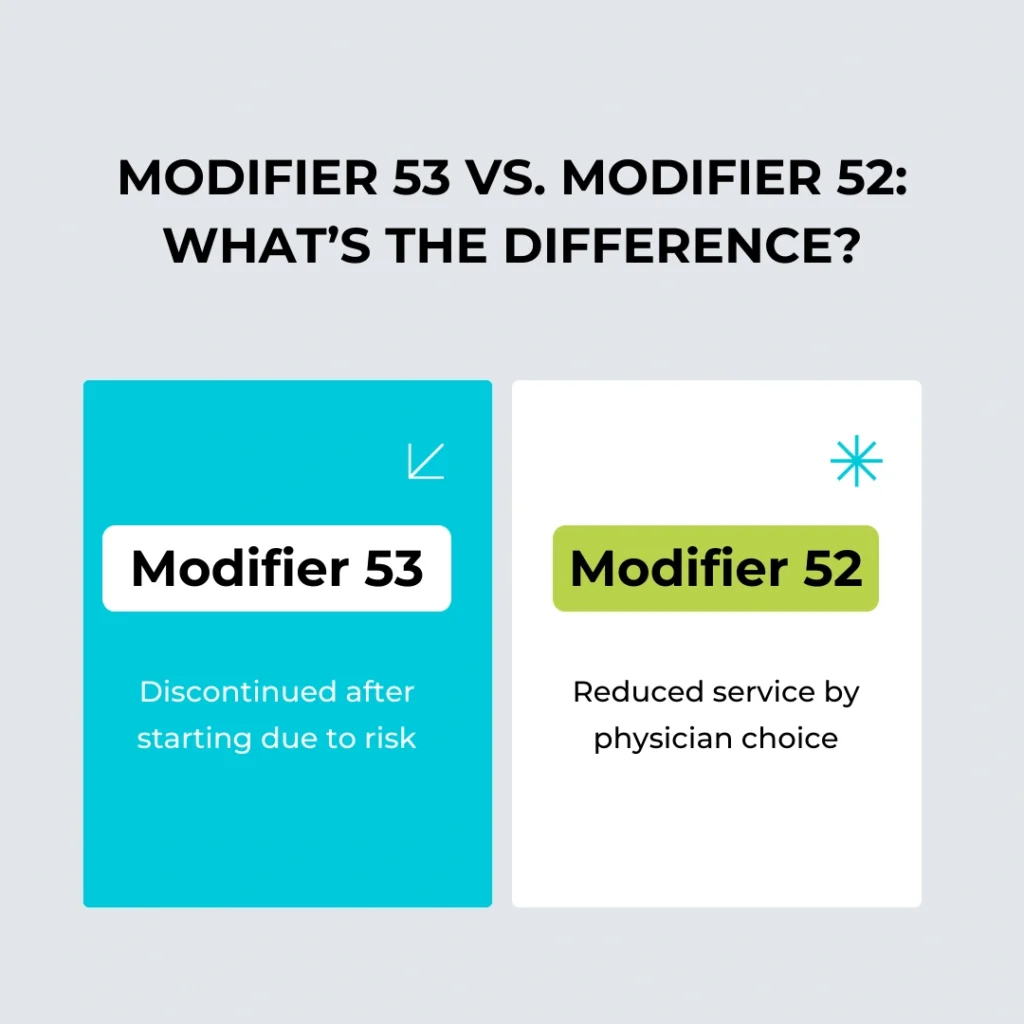
Key Differences
Both Modifier 53 and Modifier 52 deal with procedures that are not completed as originally planned, but they apply in different contexts and carry distinct billing implications.
Modifier 53: Discontinued Procedure
- Used When: A procedure is started but not completed due to extenuating circumstances, such as patient instability or complications during surgery.
- Provider Action: The physician actively terminates the procedure for the patient’s well-being.
- Example: A colonoscopy is stopped midway due to the patient experiencing severe pain or vital sign changes.
Modifier 52: Reduced Services
- Used When: A procedure or service is partially reduced in scope or complexity, often due to clinical judgment or patient-specific factors.
- Provider Action: The physician performs only part of the planned service.
- Example: A diagnostic procedure is intentionally limited because a full exam isn’t necessary or possible.
Billing Impact:
- Modifier 53 signals an unplanned discontinuation, often due to medical necessity.
- Modifier 52 reflects a planned reduction of service.
Using the correct modifier ensures that payers understand what was performed and why, helping reduce denials and improve coding accuracy.
Common Billing Mistakes
Misuse of modifier 53 can result in claim denials or audits. Watch out for these common errors:
- Appending to inappropriate codes: Some CPT codes don’t accept modifier 53
- Insufficient documentation: A sentence saying “procedure discontinued” won’t cut it
- Using instead of modifier 74 (outpatient facility modifier)
- Billing as if the procedure was completed—this is overbilling and non-compliant
Avoid these errors by using medical coding experts trained in CPT modifier protocols.
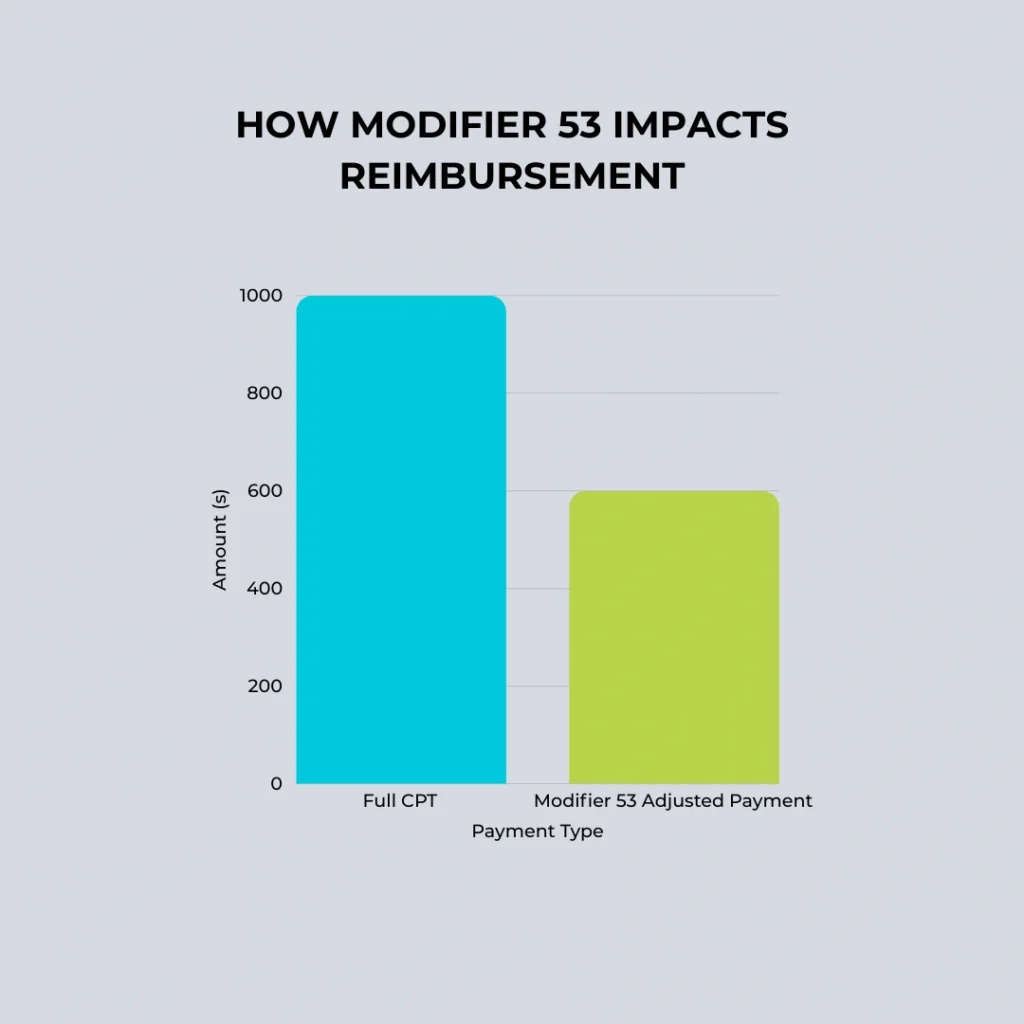
Reimbursement and Payer Policies
Reimbursement with modifier 53 depends on the payer:
- Medicare: Pays a partial amount based on services rendered before termination
- Private insurers: Vary—some require documentation submission upfront, others only on request
- Medicaid: Often has stricter modifier guidelines—check state-specific manuals
Knowing how to navigate these differences is vital for optimizing claims and avoiding rejections.
Reimbursement Workflow with Modifier 53
Best Practices for Using Modifier 53
Here are key takeaways to ensure proper modifier usage:
- Only use if the procedure has begun and patient safety is at risk
- Document everything—from initiation to reason for stopping
- Check if the CPT code is eligible for modifier 53
- Clarify distinctions between modifier 52 (reduced service) and 53 (discontinued)
- Communicate with the billing and compliance teams
Working with a medical billing company that understands these nuances can help you capture every dollar earned while staying compliant.
Conclusion
Modifier 53 is an essential tool for fair reimbursement in situations where patient safety or complications prevent procedure completion. When used appropriately with precise documentation and billing accuracy, it ensures providers are compensated for their time, effort, and clinical judgment.
Whether you’re part of a large institution or a private practice, ensures integrity in your billing and supports sustainable care delivery. Let Precision Hub help streamline your workflows with trusted revenue cycle management healthcare services tailored to your needs.
Frequently Asked Questions (FAQs)
Q1. Can I use modifier 53 for all CPT codes?
A: No. Modifier 53 is valid only for specific CPT codes check with the CPT manual or payer policy for guidance.
Q2. What’s the difference between modifier 53 and modifier 52?
A: Modifier 53 is for procedures discontinued due to risk, while modifier 52 is for reduced services completed by choice.
Q3. Will modifier 53 guarantee full reimbursement?
A: No. It generally leads to partial reimbursement based on the amount of service provided.
Q4. Do I need a separate document or just the procedure note?
A: The procedure note should be comprehensive. In some cases, a cover letter summarizing the situation can support your claim.
Q5. Should I submit photos or imaging as part of the documentation?
A: Not usually required, but it can strengthen your claim if they illustrate why the procedure was halted.