Professional wound care providers understand that accurate billing is essential to maximizing reimbursements and maintaining efficient administrative workflows. Proper use of the CPT code for wound care is critical—not only for ensuring regulatory compliance but also for enhancing financial performance. Successfully navigating the complexities of wound care coding, from debridement and dressing changes to advanced wound management, demands a precise, well-informed approach far beyond basic coding knowledge.
Partnering with a reliable medical billing company that specializes in the complexities of wound care billing is essential to achieving accurate and timely reimbursement. Such companies help eliminate costly errors and reduce claim denials, ensuring that practitioners receive proper compensation for the services rendered.
Understanding the Basics of CPT Code for Wound Care
The American Medical Association (AMA) maintains Current Procedural Terminology (CPT) codes, which serve as the standard language for reporting medical procedures. In wound care, providers use CPT codes to classify the different types of treatment they deliver to patients.
Some of the most commonly used CPT codes for wound care include:
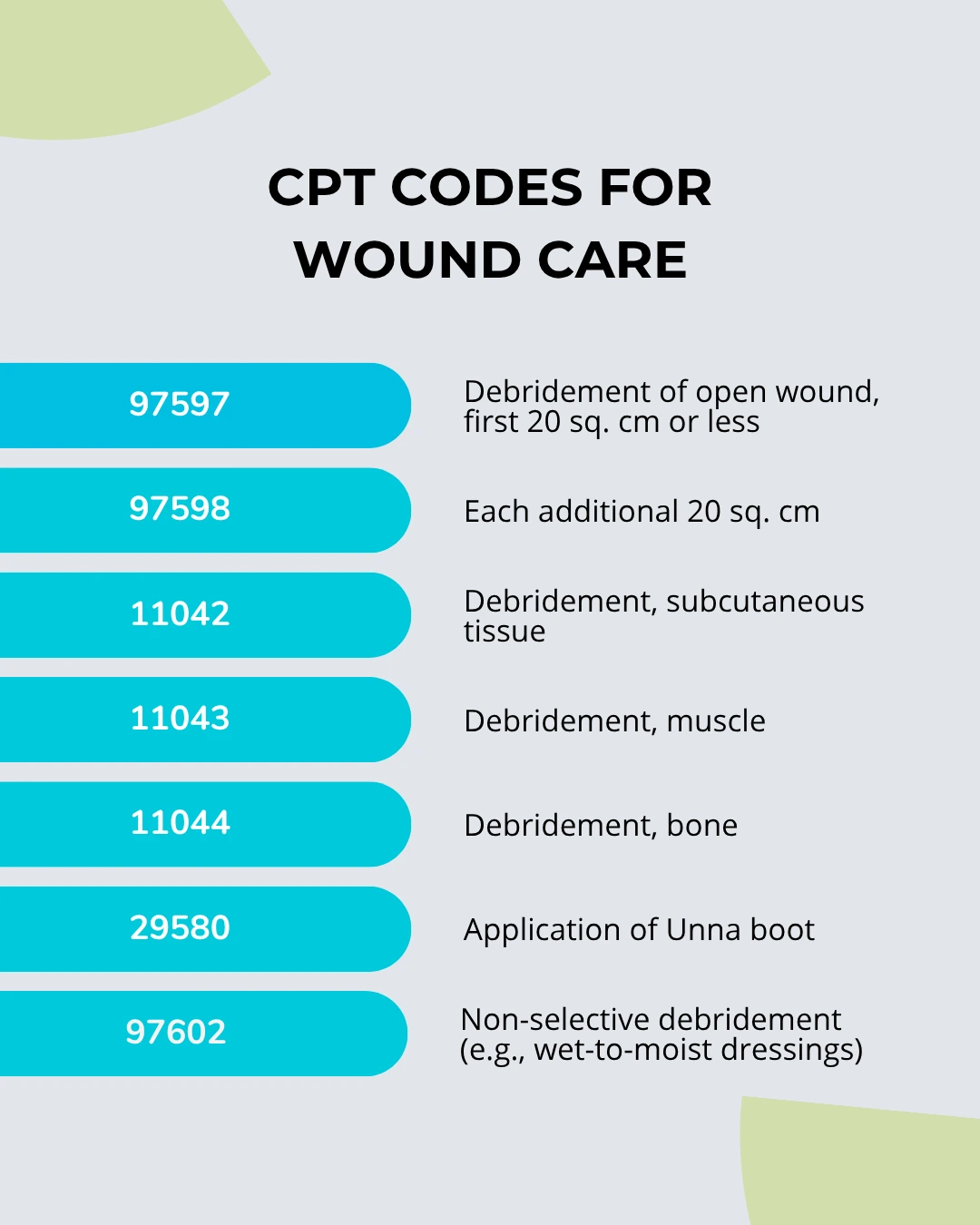
Each code reflects the depth and complexity of the wound care procedure. Using incorrect codes can lead to underbilling, overbilling, or outright claim denial.
Explore further insights read here: How to Bill for Physical Therapy Services: Understanding CPT Codes for Practitioners
Documentation Is Key
To bill accurately using any CPT code for wound care, thorough documentation is essential. Providers must include:
- Size, location, and depth of the wound
- Type of wound (acute, chronic, infected, etc.)
- Method of treatment
- Supplies and techniques used
Insurance companies closely scrutinize wound care claims, and missing details in documentation can result in delayed or denied payments. Additionally, some CPT codes require the use of modifiers to indicate bilateral procedures or additional services provided on the same day.
Incorporating solid revenue cycle management healthcare practices ensures that wound care billing begins with accurate data capture and ends with efficient claim processing.
Coding Tips for Higher Reimbursements
To maximize reimbursement, it’s important to avoid common pitfalls in wound care billing:
- Use specific codes – Select the most appropriate CPT code based on the level of service provided.
- Avoid code bundling errors – Don’t unbundle procedures that should be billed together or vice versa.
- Apply correct modifiers – Use modifiers like -59 (distinct procedural service) or -25 (significant, separately identifiable E/M service) when needed.
- Stay updated – CPT codes and payer policies change regularly. Staying informed is crucial to maintain billing accuracy.
Here’s an example: If a provider performs selective debridement on a 35 sq. cm wound, they must use 97597 for the first 20 sq. cm and 97598 for the additional 15 sq. cm. Missing the second code means losing out on additional revenue.
Common CPT Codes Used in Different Wound Care Scenarios
| CPT Code | Description | Typical Use Case |
| 97597 | Debridement (first 20 sq. cm) | Chronic ulcers, surgical wounds |
| 97602 | Non-selective debridement | Superficial wounds using wet dressings |
| 11042 | Subcutaneous debridement | Ulcers extending into subcutaneous tissue |
| 29580 | Application of Unna boot | Venous stasis ulcers |
Knowing which CPT code for wound care applies to each clinical scenario is essential for accurate billing. In some cases, codes may need to be supported by HCPCS supply codes, especially when advanced dressings or biologic products are used.
The Role of Technology in Accurate Wound Care Coding
Leveraging advanced billing software can help reduce human error and improve claims accuracy. Many modern platforms are designed to assist with proper code selection, validate documentation requirements, and provide real-time payer policy updates.
Partnering with a provider that specializes in medical billing coding can further streamline operations. These experts understand the detailed requirements of payers and can assist in auditing claims before submission, reducing denials and increasing reimbursement rates.
Avoiding Denials and Audits in Wound Care Billing
Denials often stem from:
- Incomplete or inconsistent documentation
- Incorrect CPT code usage
- Missing modifiers
- Billing for non-covered services
To avoid these, providers must implement strong internal audit processes and ensure ongoing training for billing staff. It’s also wise to periodically review payer-specific guidelines, as coverage for wound care procedures can vary widely.
Consistency and compliance are critical when billing with any CPT code for wound care. Using outdated or generic codes can trigger audits or clawbacks from payers.
Final Thoughts
Effective wound care billing relies on accurate code selection, detailed documentation, and a strong understanding of payer rules. By staying updated on CPT coding changes and employing reliable billing processes, providers can protect revenue and deliver uninterrupted care to patients.
For those seeking support, aligning with a knowledgeable medical billing company can dramatically reduce claim errors. Pair that with robust revenue cycle management healthcare strategies and a skilled medical billing coding team, and wound care providers can optimize every step of the billing process.
FAQs (Frequently Asked Questions)
1. What is the CPT code for wound debridement?
CPT codes for wound debridement include 97597, 97598, 11042, 11043, and 11044, depending on the depth and extent of the debridement.
2. Can I bill for dressing changes using CPT codes?
Routine dressing changes typically don’t qualify for billing. However, providers can use CPT code 97602 for non-selective debridement when it involves specific dressing change methods.
3. What documentation is required for wound care billing?
Clinicians must document wound size, depth, location, type of wound, and specific procedures performed. Detailed documentation supports the CPT code billed and helps prevent claim denials.
4. How often can CPT code 97597 be billed?
CPT code 97597 can be billed for each session where selective debridement is performed. Multiple sessions may be billed as long as they are medically necessary and properly documented.
5. Do wound care CPT codes require specific modifiers?
Yes. Providers apply modifiers like -59 and -25 to indicate distinct procedures or separate services performed on the same day.