Handling Medical Billing is a difficult task that includes navigating rules, guaranteeing compliance, and tracking changing reimbursement policies. Now imagine including Principal Care Management (PCM) and Chronic Care Management (CCM) into the mix. It can overwhelm you quickly, as healthcare professionals, medical coders, and billing experts all depend on an understanding of these systems to ensure correct Medicare compliance and reimbursement.
What Is Chronic Care Management (CCM)?
Medicare’s Chronic Care Management (CCM) program is designed to support patients with two or more chronic conditions expected to last at least 12 months, additionally this program offers ongoing care coordination to try to lower hospital visits while improving patient health outcomes. Moreover, it ensures that patients receive consistent and comprehensive care, ultimately leading to better management of their chronic conditions.
Who Qualifies for CCM?
CCM is designed to improve treatment for people with multiple chronic diseases. Additionally, it aims to ensure patients receive preventive care to enhance their health outcomes through continuous assistance and coordination. Furthermore, this program focuses on reducing complications and hospitalizations, ultimately promoting better long-term health management.
What Services Are Included in CCM?
It involves continuous care coordination that extends beyond in-person visits. Specifically, it includes:
- Medication management and reconciliation ensure proper treatment.
- Regular check-ins and monitoring track progress and address concerns promptly.
- Preventative health strategies reduce risks and improve long-term outcomes.
- Care coordination between multiple healthcare providers ensures seamless and comprehensive support.
Billing Time & Reimbursement
Providers must dedicate at least 20 minutes per month to non-face-to-face care coordination. As a result, Medicare reimburses for this service to encourage comprehensive patient management.
What Is Principal Care Management (PCM)?
It helps people with a single, high-risk chronic disease that requires specialized care, primarily focusing on short-term management of specific conditions to stabilize patients. Afterward, it transitions them back to their primary care providers for continued care. Additionally, this approach ensures patients receive targeted support during critical phases of their treatment.
Who Qualifies for PCM?
In 2020, Medicare introduced PCM to address gaps in chronic disease management. Specifically, PCM is designed to help people with one high-risk chronic condition that needs specialized and intense care, while CCM is for people with more than one chronic condition.
What Kinds of Services Does PCM Offer?
What Services Are Included in PCM?
Principal Care Management services include:
- Diagnosis-based treatment plans
- Frequent monitoring & symptom management
- Specialist-driven care coordination
- Comprehensive support to stabilize the condition
Billing Time & Reimbursement
PCM requires providers to dedicate at least 30 minutes per month to non-face-to-face care, which makes it a more intensive and condition-specific program compared to CCM. Additionally, this focused approach ensures patients with complex conditions receive the specialized attention they need. As a result, PCM stands out as a targeted solution for high-risk cases.
How Are PCM and CCM Different?
The scope, eligibility requirements, and billing policies of PCM and CCM are where they diverge most. Specifically, PCM is intended for patients who require specialized, short-term treatment for a single difficult ailment, whereas CCM is intended for patients who have several chronic disorders and emphasizes prevention and long-term management. By making this difference, medical professionals may tailor their treatment to the requirements of each patient, improving results for both patient groups.
Let me know if you’d like further refinements!
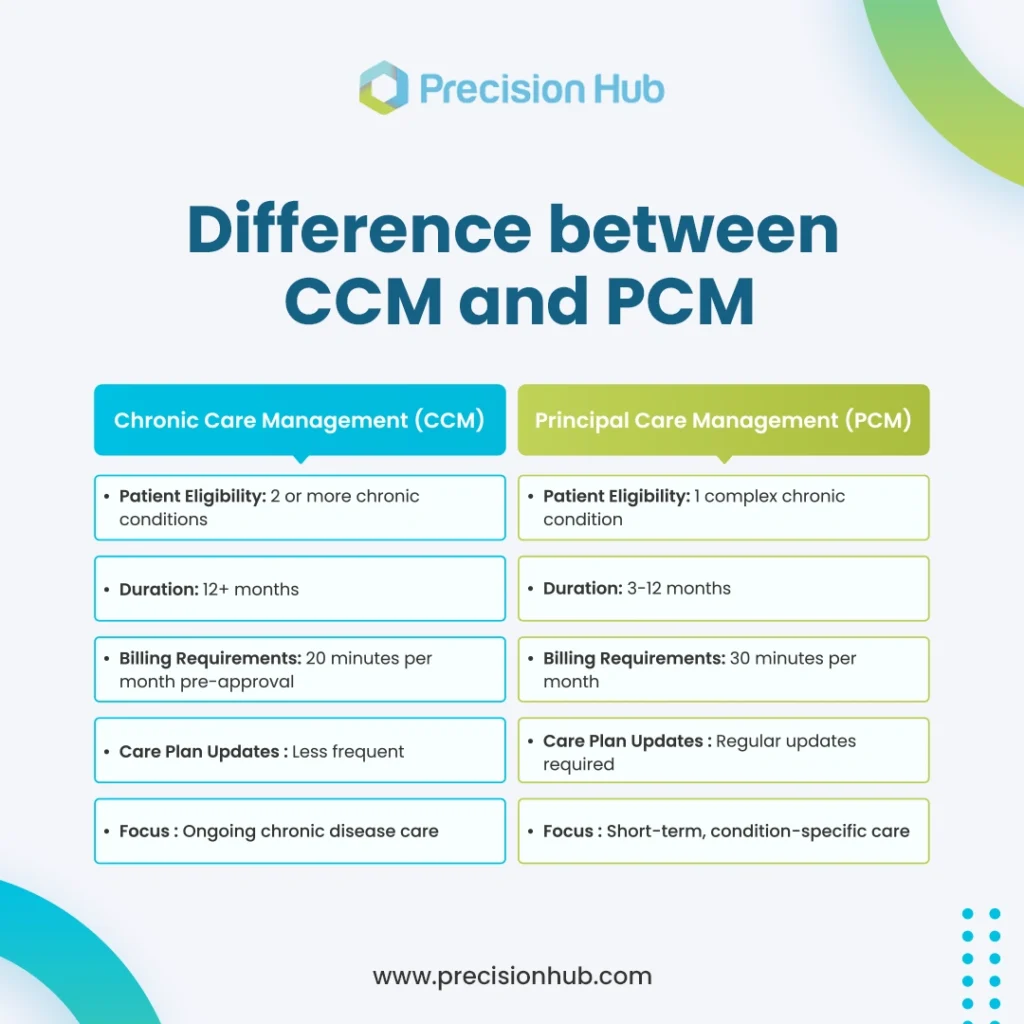
Understanding these distinctions is crucial for providers and billing specialists to ensure compliance and optimize reimbursement.
How PCM & CCM Impact Medical Billing and Coding
Proper billing and coding for PCM and CCM are critical for securing accurate payments and adhering to Medicare rules. By understanding how these programs affect medical billing, providers can avoid claim denials and maximize revenue.
Why Is Correct Billing Important?
Accurate medical billing and coding for PCM and CCM ensure maximum reimbursement and minimize claim denials. For instance, incorrect coding, incomplete documentation, or failure to meet eligibility requirements can delay payments or cause claim rejections. Moreover, these errors can lead to financial losses and administrative burdens for healthcare providers. Therefore, precision in billing and coding is essential for smooth operations.
Common PCM & CCM Billing Challenges
Navigating the complexities of PCM and CCM billing can be difficult for healthcare providers. Without proper documentation, Following Issues will occur
- Incorrect code selection can lead to claim denials.
- Inadequate documentation can delay reimbursement.
- Credentialing issues can prevent providers from enrolling in Medicare billing programs.
- Compliance requirements vary between insurers and need constant updates.
The Role of Revenue Cycle Management in PCM and CCM
How Does Revenue Cycle Management Help?
Effective revenue cycle management healthcare ensures that PCM and CCM claims, processed smoothly, leading to faster reimbursements and fewer denials. Revenue cycle management (RCM) includes:
- Patient eligibility verification
- Documentation review & claim submission
- Tracking unpaid claims & reducing denials
The Importance of Credentialing in PCM & CCM
To sign up for Medicare programs and negotiate with insurance companies, physicians must go through medical credentialing services. This process ensures that providers receive recognition and reimbursement for PCM and CCM services, thereby reducing the risk of claim denials due to enrollment issues. Additionally, it streamlines the billing process, ultimately improving efficiency and financial outcomes for healthcare practices.
Choosing the Right Program for Your Practice
Selecting the right program depends on your patients’ healthcare needs and the level of care required.
Which Program Is Right for Your Patients?
Understanding the difference between PCM and CCM is key to making informed decisions about patient care and medical billing. For instance, PCM is ideal for patients who require short-term, focused management for a single high-risk condition, while CCM is best suited for those needing long-term, ongoing care coordination for multiple chronic diseases.
How Can Providers Optimize PCM & CCM Billing?
To ensure smooth reimbursements and minimize claim denials, providers must adopt best practices for PCM and CCM billing. By following a structured approach, healthcare facilities can enhance compliance and maximize revenue.
- Accurate documentation & coding
- Staying updated on Medicare regulations
- Implementing strong revenue cycle management strategies
- Ensuring proper credentialing for seamless reimbursement
Conclusion
Choosing the appropriate program depends on patient needs, treatment duration, and the level of continuous support required. By distinguishing between PCM and CCM, healthcare providers can enhance patient care while optimizing billing practices. Additionally, both programs play essential roles in managing chronic diseases and ensuring proper Medicare reimbursement. Furthermore, understanding their differences allows providers to tailor care plans effectively, ultimately improving patient outcomes and financial efficiency.
Precision Hub: Your Trusted Billing Partner
Mastering the complexities of PCM and CCM billing allows healthcare professionals to ensure proper claims processing and maximize reimbursement.
Optimize Your PCM & CCM Billing Today!
While you concentrate on providing exceptional patient care, let Precision Hub manage your medical billing and coding. Our customized solutions enable medical professionals keep ahead of changing laws and simplify revenue cycle control. Contact us today to learn how we can support your practice’s financial success!