For many physical therapy providers, navigating the manual therapy CPT code can feel overwhelming. Using it correctly is essential—not only to stay compliant, but also to ensure timely and accurate reimbursement. If you are a small practice owner then you need to rely on medical billing services for small practices, understanding how to bill manual therapy procedures correctly helps prevent costly denials and keeps your revenue cycle running smoothly.
In this article, we’ll break down everything you need to know about the manual therapy CPT code, including how and when to use it, documentation best practices, and tips to improve your clinic’s financial performance.
What Is the Manual Therapy CPT Code?
The primary manual therapy CPT code used by physical therapists is 97140. This code covers a variety of hands-on techniques, including:
- Myofascial release
- Joint mobilization
- Manual traction
- Soft tissue mobilization
- Manipulation
These procedures must be medically necessary and aimed at restoring function, reducing pain, or improving range of motion. It’s a time-based code, meaning you must provide at least 15 minutes of manual therapy for one unit to be billable.
Explore further insights read here: Your Guide to Physical Therapy Procedure Codes: Maximizing Your Reimbursement
Proper Documentation for CPT Code 97140
Accurate documentation is critical when billing manual therapy CPT code 97140. Each note should include:
- The specific technique used
- The targeted body area
- Medical necessity for treatment
- Total time spent
- Patient response to therapy
Inadequate or vague documentation is a red flag for payers and often results in denials.
When Can You Bill Manual Therapy CPT Code?
Physical therapists can bill manual therapy CPT code 97140 when the therapy:
- Is part of an individualized treatment plan
- Requires direct, one-on-one contact
- Is not billed alongside conflicting procedures unless documented separately
One major restriction to be aware of is the mutual exclusivity with other codes like therapeutic exercise (97110) or neuromuscular reeducation (97112). You can bill both codes during the same session only if different body areas were treated, and this distinction is clearly documented.
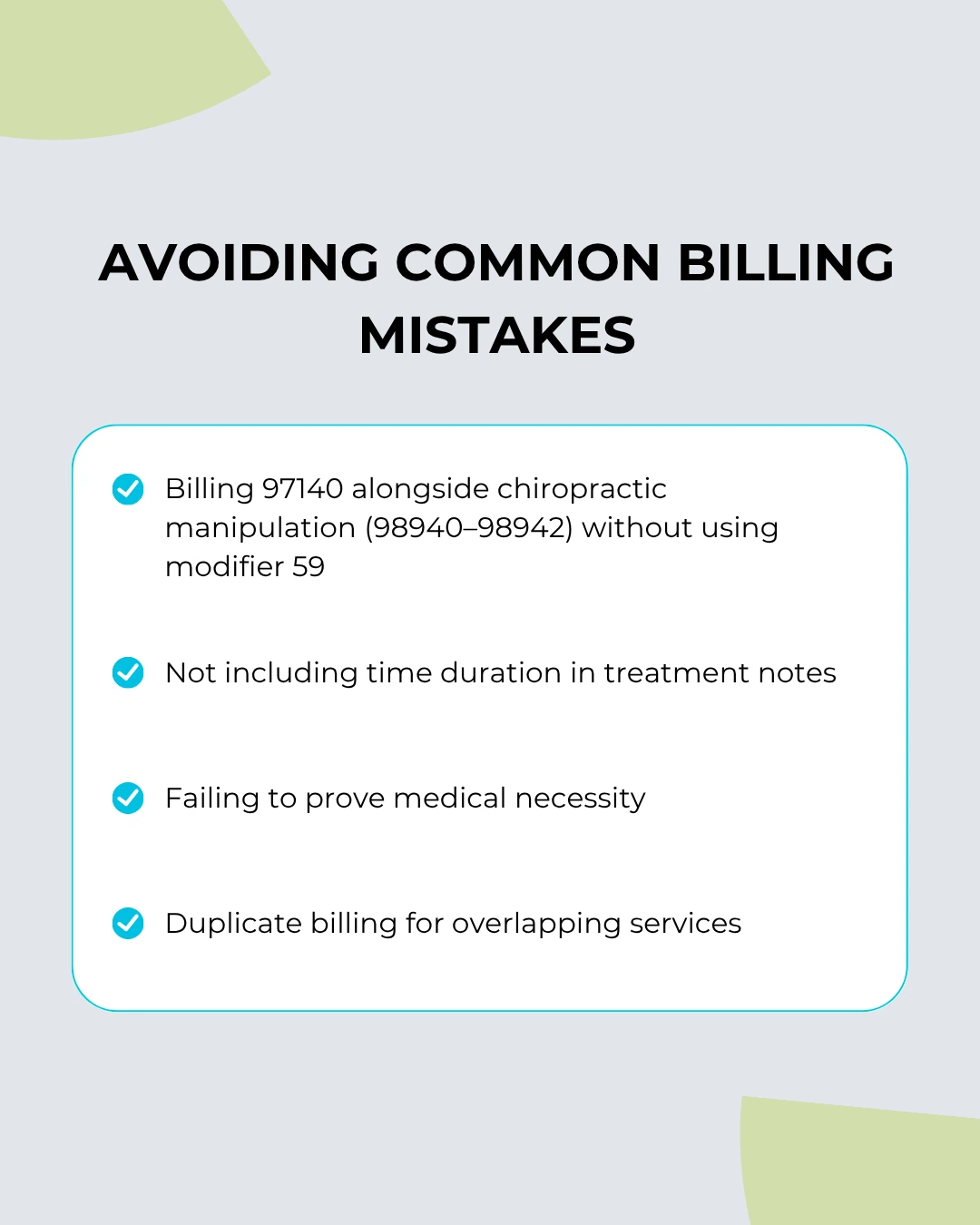
Avoiding Common Billing Mistakes
Incorrect use of the manual therapy CPT code can lead to compliance issues and denied claims. Here are common pitfalls:
Midway through improving your billing practices, consider investing in revenue cycle management services to streamline claims processing, reduce errors, and optimize reimbursements.
Manual Therapy Billing
When billing CPT code 97140 with other procedures performed during the same visit, Modifier 59 is often required to show that the services were distinct and separate. Use this modifier carefully—incorrect application can trigger audits.
For example:
- 97140 – Manual therapy for cervical spine
- 97110 – Therapeutic exercise for shoulder rehabilitation
- Use Modifier 59 on 97140 only if properly documented as a distinct procedure
Medical Necessity: What Payers Want
Payers require strong justification for manual therapy. Your notes should connect the treatment to a specific diagnosis and show how the therapy will improve the patient’s function or reduce pain. Without this, insurers may flag the manual therapy CPT code as unnecessary or experimental.
- Pain relief
- Range of motion
- Functional mobility
- Rehabilitation plan
- Manual treatment techniques
Tracking Time Accurately
Since 97140 is a timed code, make sure your EHR system tracks treatment in 15-minute increments. Under CMS guidelines, at least 8 minutes must be completed to bill one unit. More than one unit requires additional full 15-minute segments.
Example:
- 16 minutes of manual therapy = 1 unit
- 30 minutes of manual therapy = 2 units
Audit-Ready Documentation Tips
Being audit-ready saves your clinic from costly penalties. Always follow these documentation habits when using the manual therapy CPT code:
- Be detailed: “Performed joint mobilization on right knee for 15 minutes” is better than “Did manual therapy.”
- Be objective: Include measurable outcomes like improved mobility or pain reduction.
- Be time-specific: Always document the exact time spent.
Reimbursement Rates for CPT 97140
Medicare and private payer reimbursement for manual therapy CPT code 97140 varies by region and contract. On average:
- Medicare: ~$25–$30 per unit
- Commercial: $40–$60 per unit
Note that reimbursement is only made when documentation and modifier usage are appropriate. It’s a smart move to regularly review payer guidelines and fee schedules.
If your clinic struggles with complex payer rules, consider outsourcing to a medical billing and coding company to handle coding accuracy and compliance.
Boosting Revenue Through Proper Coding
Optimizing how you use the manual therapy CPT code can increase your clinic’s bottom line. By documenting thoroughly, using modifiers correctly, and billing distinct services accurately, you can avoid underpayments and denials.
Stay educated, audit your claims regularly, and use tools or services to ensure every session is billed at its full value.
Final Thoughts
Mastering the manual therapy CPT code is essential for physical therapy practices looking to stay compliant and financially healthy. It’s not just about billing—it’s about accurate clinical representation and value-driven care. From documentation to modifiers, every detail counts.
If you’re a clinic owner or provider looking to improve your billing process, Precision Hub offers expert support tailored to the unique needs of physical therapy practices. Whether you’re aiming for better compliance or more consistent reimbursements, our team is here to help you navigate the complexities of billing and stay ahead of industry changes.
FAQs (Frequently Asked Questions)
Q1. What is the manual therapy CPT code?
The manual therapy CPT code is 97140, used for hands-on treatments like joint mobilization, myofascial release, and soft tissue work.
Q2. Can I bill CPT 97140 and 97110 together?
Yes, but only if the procedures are performed on different body areas and properly documented. Modifier 59 may be required.
Q3. How much time is needed to bill one unit of CPT 97140?
At least 15 minutes is needed, with a minimum of 8 minutes to bill one unit under Medicare’s 8-minute rule.
Q4. What documentation is required for manual therapy billing?
Notes must include the technique, body part treated, time spent, and the reason the therapy was medically necessary.
Q5. Why do insurance claims for 97140 get denied?
Common reasons include insufficient documentation, missing modifiers, or billing conflicting codes without proper separation.