Accurate coding plays a pivotal role in securing proper reimbursement within the complex healthcare landscape. One area that often leads to confusion for healthcare providers and billing professionals is the use of specific modifiers. Gaining a clear understanding of their purpose, proper application, and common billing scenarios is key to ensuring accurate claims and avoiding costly denials.
What Is Modifier 26?
Modifier 26 is used in medical billing to indicate the professional component of a service. Many diagnostic services, particularly those involving imaging or laboratory work, consist of two parts: the technical component and the professional component. While the technical component covers the equipment, supplies, and technician’s time, the professional component refers to the physician’s work—such as interpreting results or providing a written report.
For example, when a radiologist interprets an X-ray taken at an outpatient facility, the billing should reflect only the interpretation and report, not the cost of performing the test itself.
Medical billing company professionals regularly differentiate between shared services to ensure precise documentation and reimbursement. Misusing this modifier can lead to overbilling or claim rejections, ultimately affecting revenue flow.
When to Use Modifier 26
Modifier 26 is applicable in situations where a healthcare provider only performs the professional component of a procedure. This typically includes diagnostic imaging such as:
- CT scans
- MRIs
- X-rays
- ECGs or EEGs
Let’s say a physician reviews an echocardiogram performed at a separate facility. The facility bills for the technical portion, while the physician bills with Modifier 26 to reflect only the interpretation. This ensures that both parties are paid appropriately for their roles.
You should attach Modifier 26 to the appropriate CPT code only if:
- The provider is not billing for the technical component.
- The service is not performed in a facility that includes both components in one global fee.
- The CPT code has both a technical and professional component.
Modifier 26 should not be used on codes that do not split into components or in cases where the provider performed both aspects of the service.
Looking more details? Keep going: EMR vs. EHR: What’s Best for Your Healthcare Practice
Proper Documentation Matters
Accurate documentation is essential when using Modifier 26. The provider’s notes should clearly reflect their professional contribution, including the interpretation and analysis of the service performed. This is especially critical during audits or claim reviews. Lack of clarity in documentation can result in delayed payments or denials.
In the context of revenue cycle management healthcare, proper use of Modifier 26 plays a crucial role. When combined with accurate coding and timely claim submissions, it helps ensure a seamless billing process that improves cash flow and minimizes administrative overhead.
Common Scenarios for Modifier 26 Usage
- Radiology Services: A radiologist reviews and interprets an X-ray taken at an imaging center. Since the imaging center owns the equipment and handles the technical part, the radiologist bills only for their report.
- Cardiology Studies: A cardiologist interprets an ECG performed at a hospital. The hospital bills for the technical part; the cardiologist bills for the professional analysis.
- Pathology Reviews: A pathologist reviews a tissue sample slide prepared in a lab. The lab bills the technical component; the pathologist bills the professional component.
Avoiding Common Errors
Modifier 26 errors can have financial consequences. Here are some mistakes to avoid:
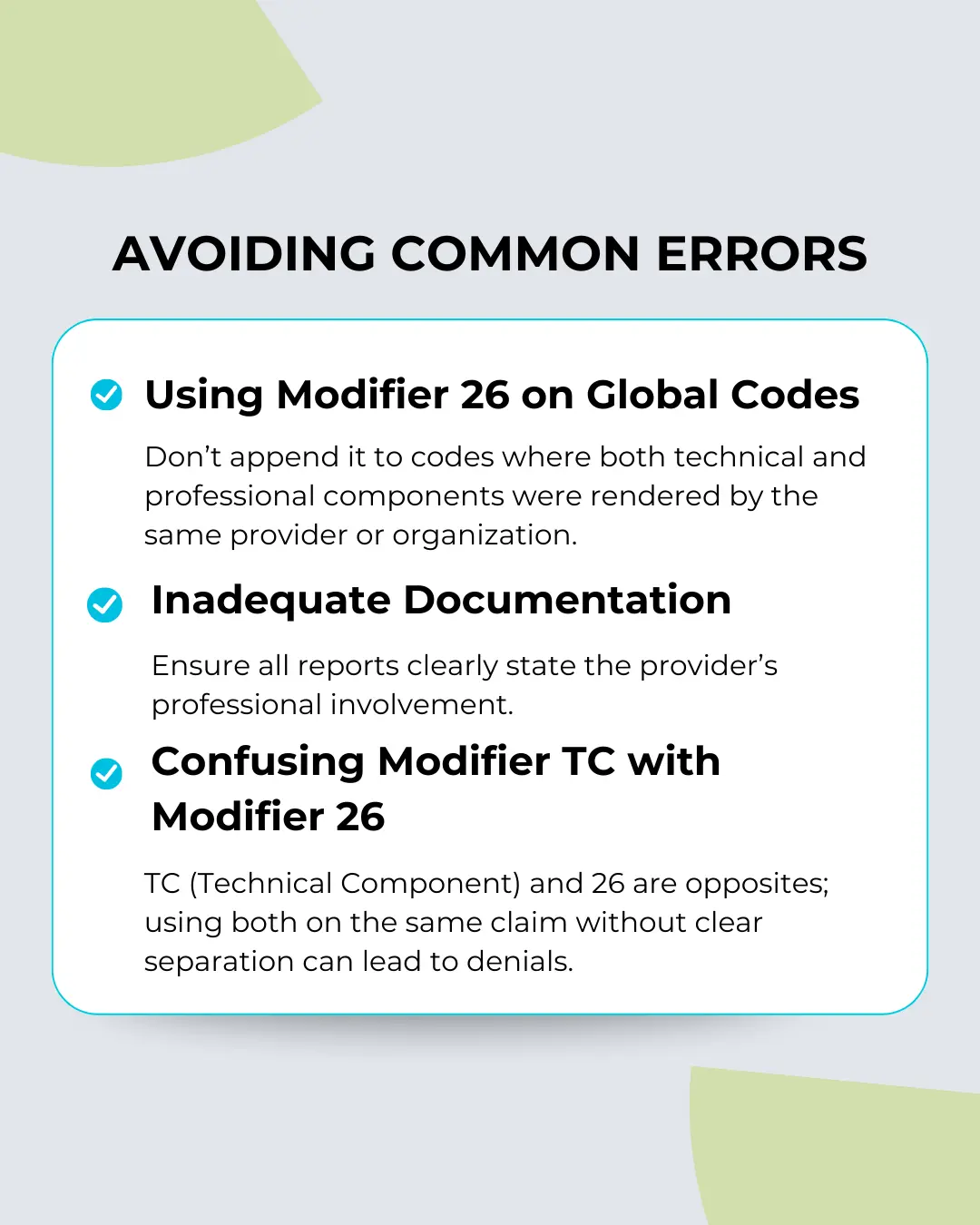
Midway through your billing processes, training your staff or outsourcing to a qualified medical billing coding expert can drastically reduce the likelihood of such errors. Accuracy in modifiers not only affects reimbursement but can also impact compliance.
Global vs. Split Billing: Knowing the Difference
Understanding the difference between global billing and split billing is essential for correct Modifier 26 usage. Global billing occurs when the same provider or entity performs both components of a service, meaning no modifier is necessary. Split billing happens when the service is shared, and modifiers like 26 (professional) and TC (technical) are used to distinguish the services.
For example, in a hospital setting where a physician interprets a scan conducted by the hospital’s equipment and staff, the billing must be split. The physician bills for the professional component, and the hospital uses Modifier TC.
It’s also important to know that not all CPT codes are eligible for this type of split billing. Always refer to the CPT codebook or payer guidelines before appending any modifiers.
Payer Policies and Reimbursement Impacts
Insurance payers may have specific rules regarding Modifier 26. Medicare, for instance, allows the modifier on certain codes but not others. Some private payers might require additional documentation or prior authorization when modifiers are used. Verifying with each payer helps prevent delays and improves reimbursement rates.
Incorporating thorough payer-specific protocols into your billing workflow can be a game-changer. For this reason, aligning with a reliable team can ensure consistency, minimize rework, and keep your billing department compliant with ever-changing regulations.
Final Thoughts on Using Modifier 26 Correctly
Using this modifier may seem straightforward, but consistent accuracy requires expertise, training, and up-to-date knowledge of coding guidelines. When used correctly, it protects providers from lost revenue and ensures fair reimbursement for their professional services.
In the end, understanding the importance of modifiers is about more than billing—it’s about streamlining workflows, maintaining compliance, and enhancing overall operational efficiency. With healthcare regulations continuing to evolve, investing in solid (RCM) healthcare strategies—including correct modifier usage—is a must for any thriving practice or facility.
Would you like a checklist or downloadable guide on when to use Modifier 26?
FAQS (Frequently Asked Questions)
1. What is the professional component in medical billing?
The professional component indicates the interpretation or report generation of a service when the technical portion is performed elsewhere.
2. When should the professional component be used?
It is used when a provider only performs the professional component of a service, such as interpreting diagnostic tests or results.
3. Can the professional component be applied to all CPT codes?
No, it is only applicable to CPT codes that have both technical and professional components, like imaging or lab tests.
4. How does the professional component differ from the technical component?
The professional component covers the interpretation, while the technical component applies to the equipment and personnel involved.
5. Can the professional component be used if the physician owns the equipment?
No, if the physician owns the equipment, the entire service is billed as a global charge without needing the professional component.