It’s crucial to apply the correct codes and modifiers to ensure accurate reimbursement and compliance. One commonly misunderstood modifier is modifier 51, which is used when multiple procedures are performed during the same session. This modifier helps avoid billing mistakes and ensures that healthcare providers are paid fairly for all the services they provide. Whether you are a healthcare provider or a member of a revenue cycle management team, is essential for accurate coding and successful claim submissions.
The documentation required to support its application, and common mistakes to avoid. Additionally, we will share best practices to guide you in managing billing services medical procedures while ensuring compliance with coding standards.
What Is Modifier 51?
Modifier 51 is a CPT (Current Procedural Terminology) modifier used when a provider performs multiple procedures in a single session. This modifier indicates that a particular service or procedure is secondary and should be reimbursed at a reduced rate, typically used in situations where multiple procedures are necessary but not mutually exclusive, meaning they don’t overlap or negate the need for the other.
For example, if a patient undergoes a diagnostic colonoscopy and a biopsy during the same visit, 51 modifier would be used to show that these are distinct but related services and ensures that both procedures are reimbursed but that the second procedure is billed at a reduced rate, as is standard practice when multiple procedures are performed together.
When to Use
It depends on specific conditions and the type of procedure performed. Here’s a breakdown:
Valid Uses of Modifier 51
- Multiple unrelated procedures: When more than one distinct procedure is performed in a single session, such as a colonoscopy and a biopsy, indicates these services should be billed separately but at a reduced rate.
- Multiple procedures from the same specialty: For example, a patient undergoing two different orthopedic surgeries (such as repairing two fractures) may require 51 modifier to reflect that these are separate procedures.
- Two or more different procedures on the same anatomical site: In some cases, performing more than one procedure on the same body part requires to show that these services should be billed separately.
Invalid Uses of Modifier 51
- Routine procedures with no significant variation: Some procedures, like simple lab tests or common imaging, don’t require because they’re routinely performed and don’t involve significant variations.
- Multiple procedures that are considered bundled: If a series of procedures are grouped under a single code, 51 modifier should not be used. These bundled services are already considered one unit of care.
- Repetitive procedures: If a procedure is repeated due to patient non-compliance or other unrelated factors, modifier 51 is inappropriate.
To ensure 51 modifier is applied correctly, medical billing teams must closely examine the specific procedures involved and verify that they meet the criteria for this modifier.
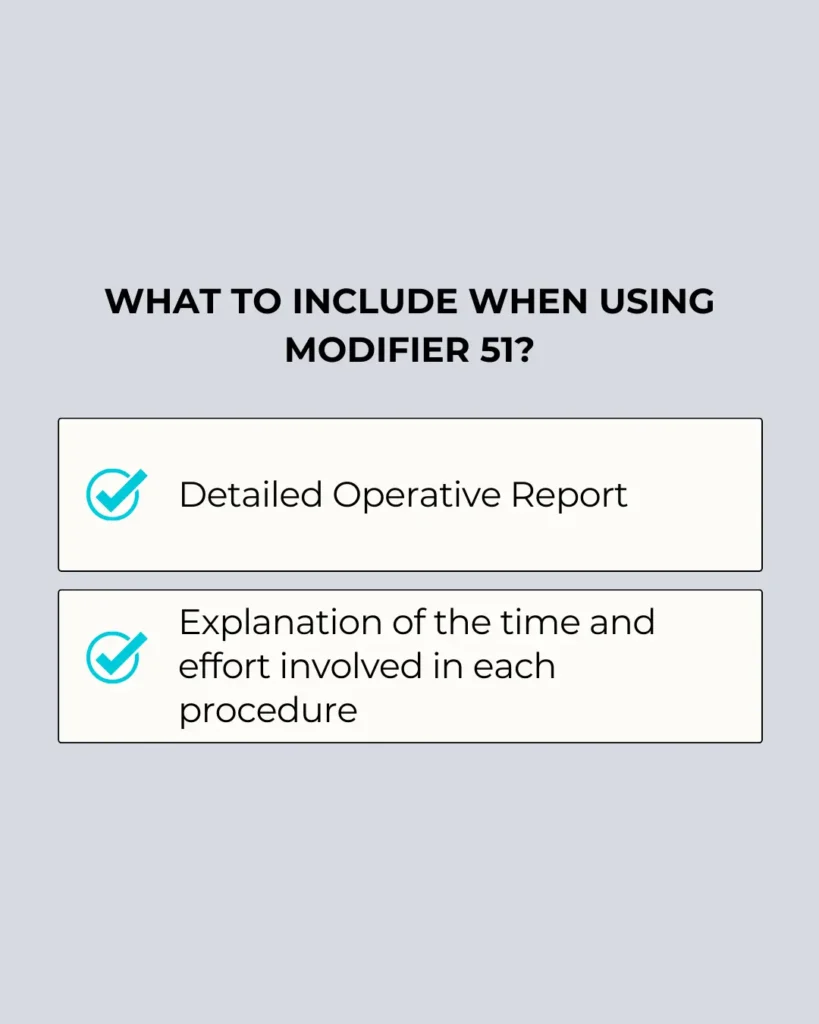
Documentation Requirements for Modifier 51
Accurate documentation is essential when using modifier 51. Without the proper documentation, your claim may be rejected, and you may miss out on the reimbursement you’re entitled to. The following documentation is required:
- Operative report: The report should clearly state the procedures performed, including the reason for each procedure and the time spent on each.
- Description of the procedures: Provide a detailed description of the secondary procedures and explain why each one is necessary.
- Time and resources: Document the time spent on each procedure to justify that the procedures were distinct and required separate billing.
Common Mistakes to Avoid with Modifier 51
Even though modifier 51 is a vital tool for accurate billing, it’s often misused. Here are some common mistakes to avoid:
- Incorrectly using 51 modifier: 51 Modifier should only be applied when two or more procedures are performed in a single session. It should not be used when the procedures are bundled or considered part of the same service.
- Failing to document thoroughly: Inadequate documentation can result in claim denials. Always ensure that your documentation supports the use of 51 modifier.
- Misunderstanding payer policies: Different payers have varying rules about when 51 modifier can be used. Be sure to review payer-specific guidelines before submitting claims.
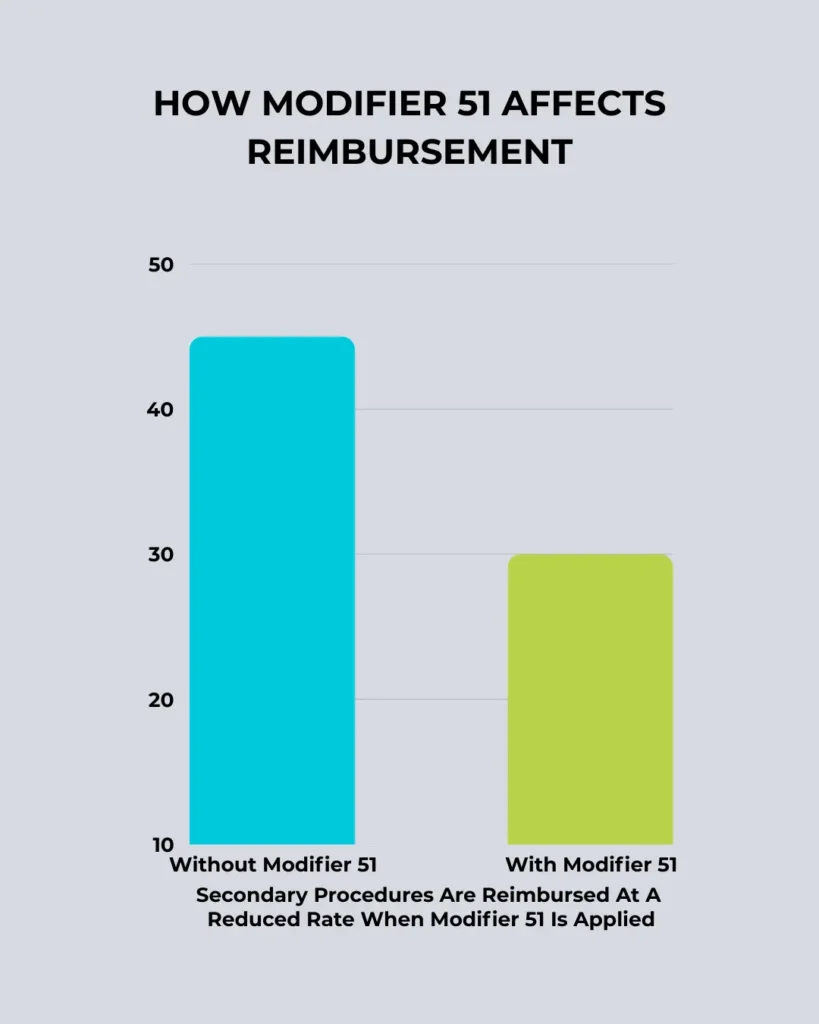
The Financial Impact of Modifier 51
Modifier 51 impacts the financial outcome of multiple-procedure claims by reducing reimbursement for secondary procedures. However, when applied correctly, 51 modifier ensures healthcare providers are compensated for the extra work involved. Here’s how it affects the payment structure:
- Primary procedure: The first procedure performed is reimbursed at the full rate.
- Secondary procedures: Additional procedures are reimbursed at a reduced rate, typically 50-75% of the full rate.
Despite the reduction in payment, modifier 51 is crucial for ensuring that healthcare providers are reimbursed for all services provided. For more on how to optimize reimbursement, understanding the nuances of healthcare revenue cycle management is key.
Documentation Requirements
The Financial Impact
Read more about: How To Choose the Best Medical Billing Service Provider
Best Practices for Using Modifier 51
Here are some best practices for ensuring modifier 51 is used correctly:
- Understand payer policies: Always check the guidelines for each payer to ensure that modifier 51 is applied by their rules.
- Use modifiers consistently: Apply only when necessary, and don’t overuse it for bundled or routine procedures.
- Document all procedures: Provide thorough documentation that explains the need for each procedure performed.
- Communicate with coding teams: Regularly review coding practices and communicate any changes in procedure types or guidelines to the medical coding team.
Conclusion
Modifier 51 is an essential tool in medical billing coding, particularly for providers who perform multiple procedures in a single session. When used correctly, it helps ensure that healthcare providers are fairly reimbursed for all services rendered. Proper documentation, understanding payer policies, and avoiding common mistakes are critical steps in making sure 51 modifier is used accurately.
If you need assistance with billing services, medical or healthcare revenue cycle management, working with a professional coding partner can help optimize your billing processes and ensure compliance. By adhering to proper coding practices, your practice can maximize reimbursement and minimize errors.
FAQs About Modifier 51
Q1. Can I use for any CPT code?
A: No. is valid only for specific CPT codes. Always check with the CPT manual or payer policy for eligibility.
Q2. What’s the difference between modifier 51 and modifier 52?
A: Modifier 51 is used for multiple procedures, while modifier 52 is for reduced services when the procedure is performed but not to the full extent.
Q3. Will using affect reimbursement rates?
A: Yes, typically results in a reduced payment for secondary procedures performed in the same session.
Q4. Can 51 modifier be used for cosmetic procedures?
A: 51 Modifier is not typically used for cosmetic procedures unless multiple procedures are performed on the same patient during the same session.