In today’s complex and tightly regulated landscape of medical billing, accuracy is critical for ensuring compliance, minimizing claim denials, and securing appropriate reimbursement. Proper application of billing modifiers is a key component of this process, and among them, the 79 modifier serves a distinct and essential function in identifying services that warrant separate payment during the postoperative period.
Understanding how to use it properly is especially important for small clinics, surgical practices, and any facility that performs procedures classified as major surgeries. Healthcare organizations that provide medical billing services for small practices should be especially diligent about educating staff on the requirements surrounding this important modifier.
What Is Modifier 57?
Modifier 57 is defined by the American Medical Association (AMA) as indicating that the “decision for surgery” was made during the E/M service. It should only be appended to an E/M code when the decision to perform a major surgical procedure—one with a 90-day global period—is made during that visit.
This distinction is critical for proper billing. Without it, the E/M service could be bundled with the surgical procedure, resulting in lost reimbursement. Adding the appropriate modifier informs the payer that the E/M visit was medically necessary and separate from the typical preoperative care included in the surgery’s global package.
Let’s say a patient visits a surgeon for abdominal pain. After a thorough exam and diagnostic imaging, the provider determines the patient needs an emergency appendectomy. Because the decision for surgery was made during that encounter, the modifier should be appended to the E/M code on the claim.
When to Use Modifier 57
To ensure accurate and compliant billing, modifier 57 should be used only when the following conditions are met:
- The procedure being performed is considered major surgery (90-day global period).
- The decision to proceed with surgery is made during the E/M service.
- The E/M service is significant, separate, and medically necessary.
If any of these elements are missing, the modifier should not be used. It is also important to note that this modifier does not apply to minor procedures (0- or 10-day global periods). For those, providers may need to consider using a different modifier instead.
For example, a patient comes in with a torn meniscus. The orthopedist evaluates the condition, recommends arthroscopic surgery the same day, and schedules the procedure. Because this is a major surgery and the decision was made at that visit, modifier 57 is appropriate.
Modifier 57 vs. Modifier 25: Know the Difference
One of the most common mistakes in medical billing is confusing modifier 57 with modifier 25. While both modifiers are used to indicate that an E/M service is separate and distinct from a procedure, they apply in different situations:
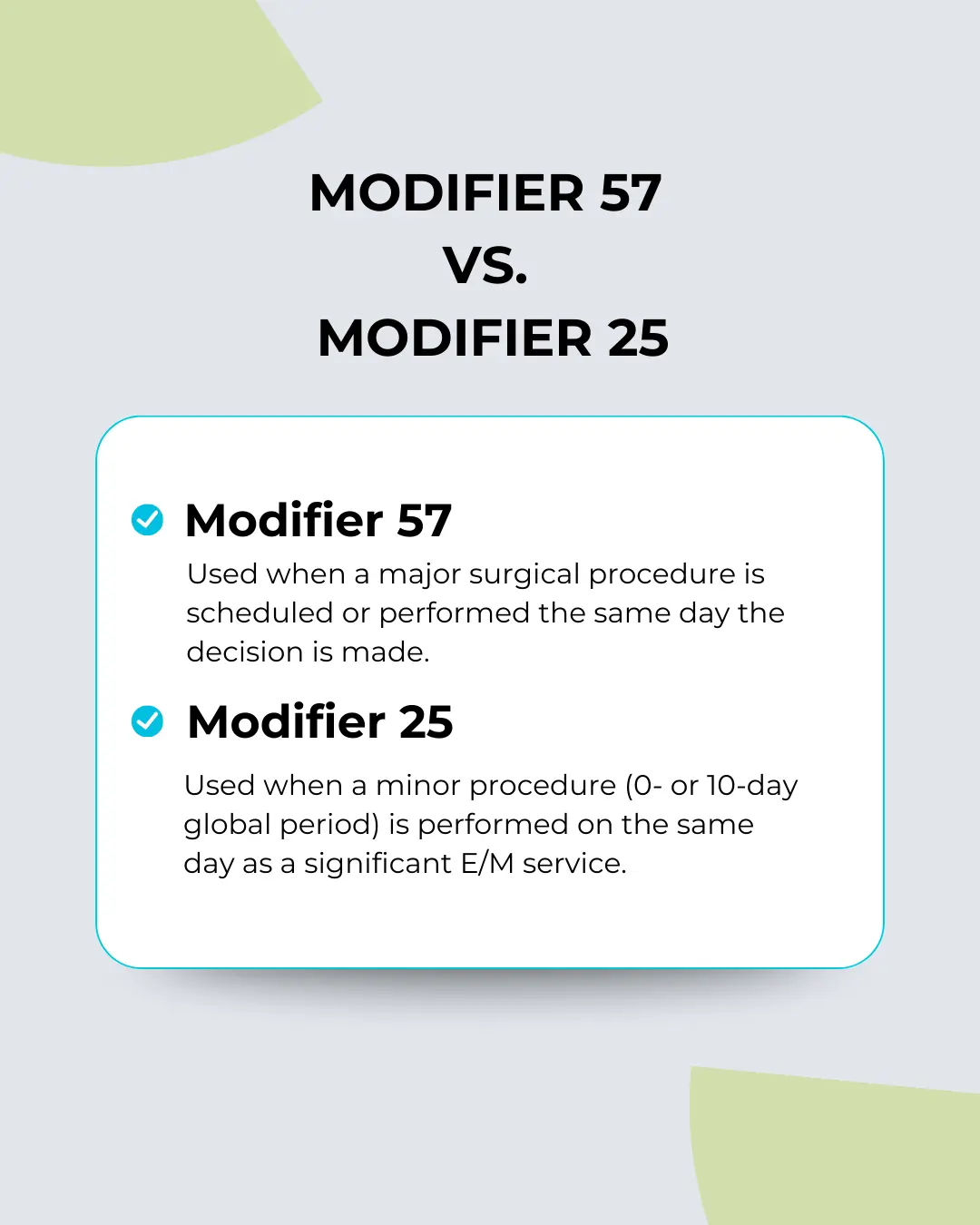
Understanding the correct use of each modifier is essential for coders and billing professionals. Practices that rely on RCM Services should verify that their teams are properly trained on how to distinguish between these modifiers to reduce rework and denials.
Common Mistakes When Using Modifier 57
Using modifier 57 incorrectly can lead to a host of billing problems. Here are some of the most common errors:
- Applying It to Minor Procedures
This is a frequent mistake. If the procedure has a 0- or 10-day global period, the modifier should not be used. Instead, consider whether modifier 25 is more appropriate. - Lack of Proper Documentation
Payers need to see that the decision for surgery was made during the E/M service. If the documentation doesn’t clearly support this, the E/M service may be denied. - Automatic Modifier Usage
Some billing teams automatically apply it whenever a surgery is performed on the same day as an office visit. However, if the decision was made before the visit, using the modifier is not appropriate.
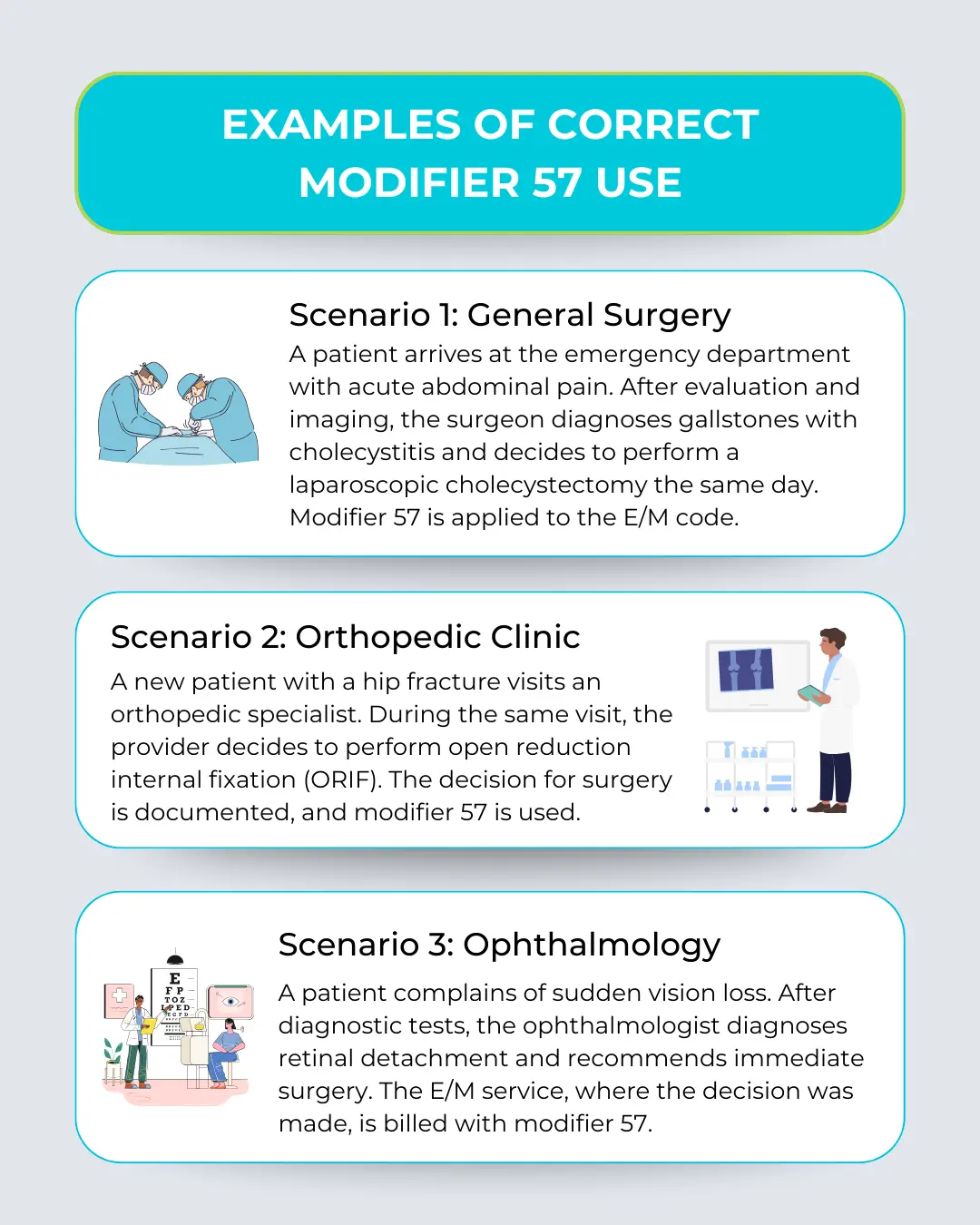
Examples of Correct Modifier 57 Use
Here are a few practical examples to illustrate proper usage:
Documentation Best Practices
Using modifier 57 successfully depends heavily on documentation. The medical record should include:
- Patient’s presenting symptoms or condition
- Examination findings
- Diagnostic results
- Clinical reasoning behind the surgical recommendation
- The provider’s decision-making process
This level of detail helps substantiate the separate nature of the E/M visit and supports the claim in case of audits. Clinics offering medical billing coding services must consistently review documentation for modifier usage accuracy.
Payer-Specific Considerations
Different payers may have specific expectations for how modifier 57 is used. Medicare and many private insurers recognize the modifier but may require detailed documentation or impose policy-specific rules.
Always check payer policies when submitting claims with modifier 57 to avoid unexpected denials. Some insurers may reject the E/M code if they believe the visit was routine or lacks documentation of the surgical decision.
Tips for Success with Modifier 57
To improve modifier accuracy and protect your revenue, consider these best practices:
- Educate providers: Help clinicians understand when and how to use modifier 57.
- Use EMR alerts: Build rules in your EHR system to flag when modifier 57 may be appropriate.
- Audit claims regularly: Check for correct use of modifiers and proper documentation.
- Partner with experts: Working with specialists in medical billing services for small practices can streamline compliance and improve collections.
Final Thoughts
Correctly using modifier 57 ensures providers are reimbursed for E/M services that result in surgical decisions. It separates a medically necessary evaluation from the procedure itself, highlighting the value of clinical judgment made during the visit.
While the rules are clear, execution can be tricky. Modifier misuse often leads to denials, delays, and compliance risks. By maintaining strong documentation, understanding surgical global periods, and training staff appropriately, your practice can avoid common pitfalls.
For busy providers, parnering with experts can take the burden off internal teams while improving accuracy. Don’t let a small code cost your practice big money—make modifier 57 part of your billing strategy done right.