Modifier 58 is one of those specific CPT modifiers that ensures proper reimbursement when a staged or related procedure is performed during the postoperative period. It plays a critical role in how payers assess whether a subsequent procedure falls under the global surgical package or qualifies for separate payment.
Understanding modifier 58 is key to avoiding claim denials, ensuring compliance, and supporting the financial health of your medical billing service. Whether you’re a seasoned coder or someone involved in healthcare operations, having a clear grasp of this modifier can make all the difference.
What Is Modifier 58?
Modifier 58 is defined by the American Medical Association (AMA) as a “staged or related procedure or service by the same physician or other qualified healthcare professional during the postoperative period.” It’s appended to CPT codes when a subsequent procedure:
- Was planned prospectively (at the time of the original procedure),
- Is more extensive than the original procedure, or
- Is for therapy following a diagnostic surgical procedure.
Unlike other modifiers, such as 78 or 79, modifier 58 specifically indicates that the next procedure is not unexpected or unrelated—it was either scheduled in advance or is a logical next step in treatment.
When to Use Modifier 58
To use modifier 58 appropriately, the following conditions must be met:
- Same Physician: The staged or related procedure must be performed by the same physician or a provider in the same group practice.
- Postoperative Period: The new procedure occurs within the global period of the original surgery.
- Staged or Related: The procedure must be documented as planned or related at the time of the initial surgery.
Common Scenarios for Modifier 58
- A plastic surgeon removes a tumor and schedules reconstructive surgery a few weeks later.
- An orthopedic surgeon repairs a fractured bone and then returns to remove surgical pins.
- A general surgeon performs a biopsy and later completes a definitive cancer resection.
In these cases, modifier 58 signals that the follow-up procedure is necessary and part of a staged treatment plan, which typically results in full payment, rather than being bundled into the initial global surgical package.
See more details? How To Improve Patient Payment Collection Rates
Modifier 58 vs. 78 vs. 79
Misuse of modifiers is one of the leading causes of denied claims. It’s critical to distinguish modifier 58 from similar modifiers like modifier 78 and modifier 79:
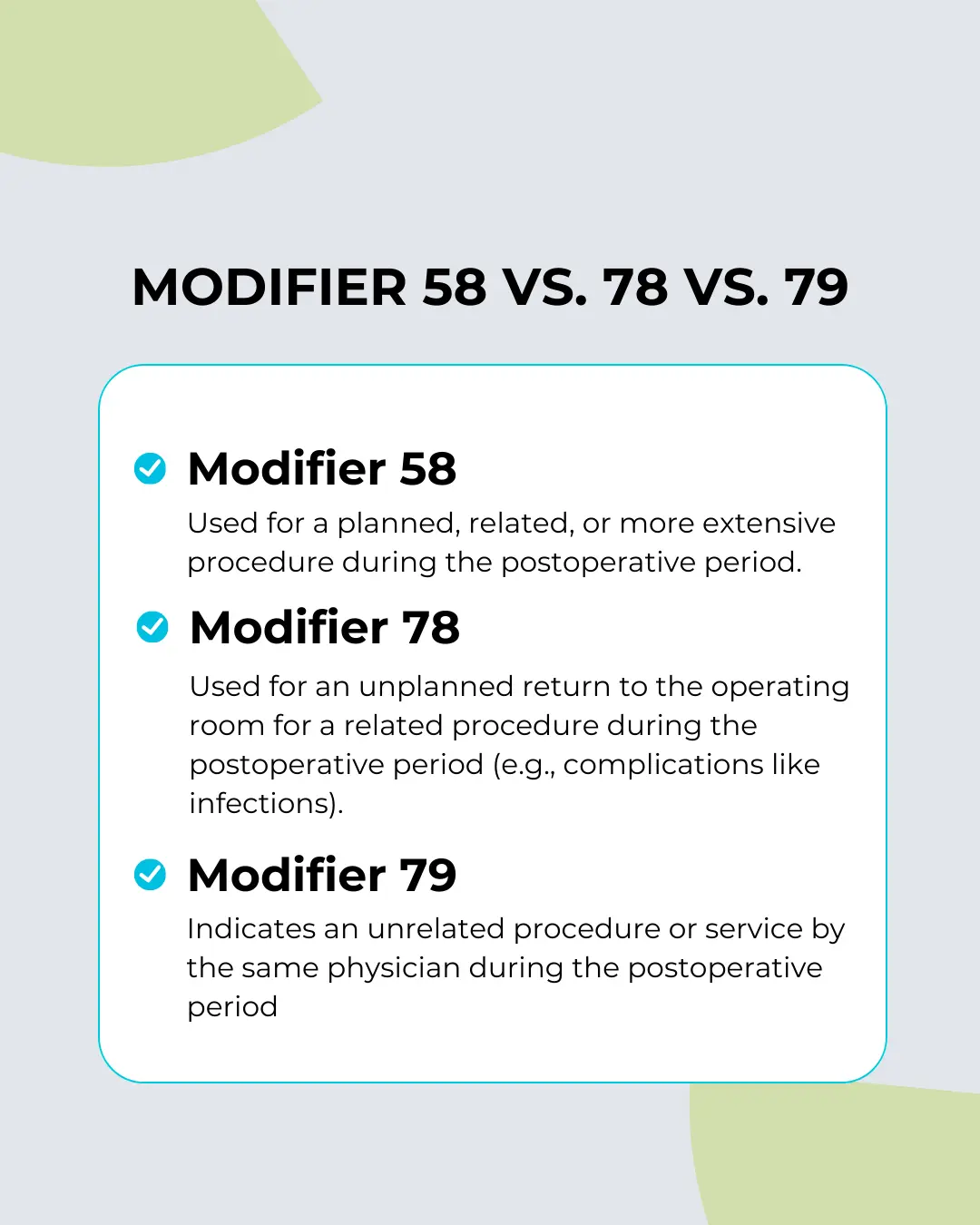
The key takeaway is that it is used for planned, related, or more extensive procedures, not for emergencies or unrelated follow-ups.
Documentation Requirements
Clear and precise documentation is essential when using it. Coders and billers must ensure the physician’s notes support the staged or related nature of the procedure. The documentation should include:
- Details of the original procedure
- Notation of the staged or planned future procedure
- Explanation of the medical necessity for the follow-up
Accurate documentation helps prevent audits, supports proper claim submission, and streamlines the entire Revenue Cycle Management process.
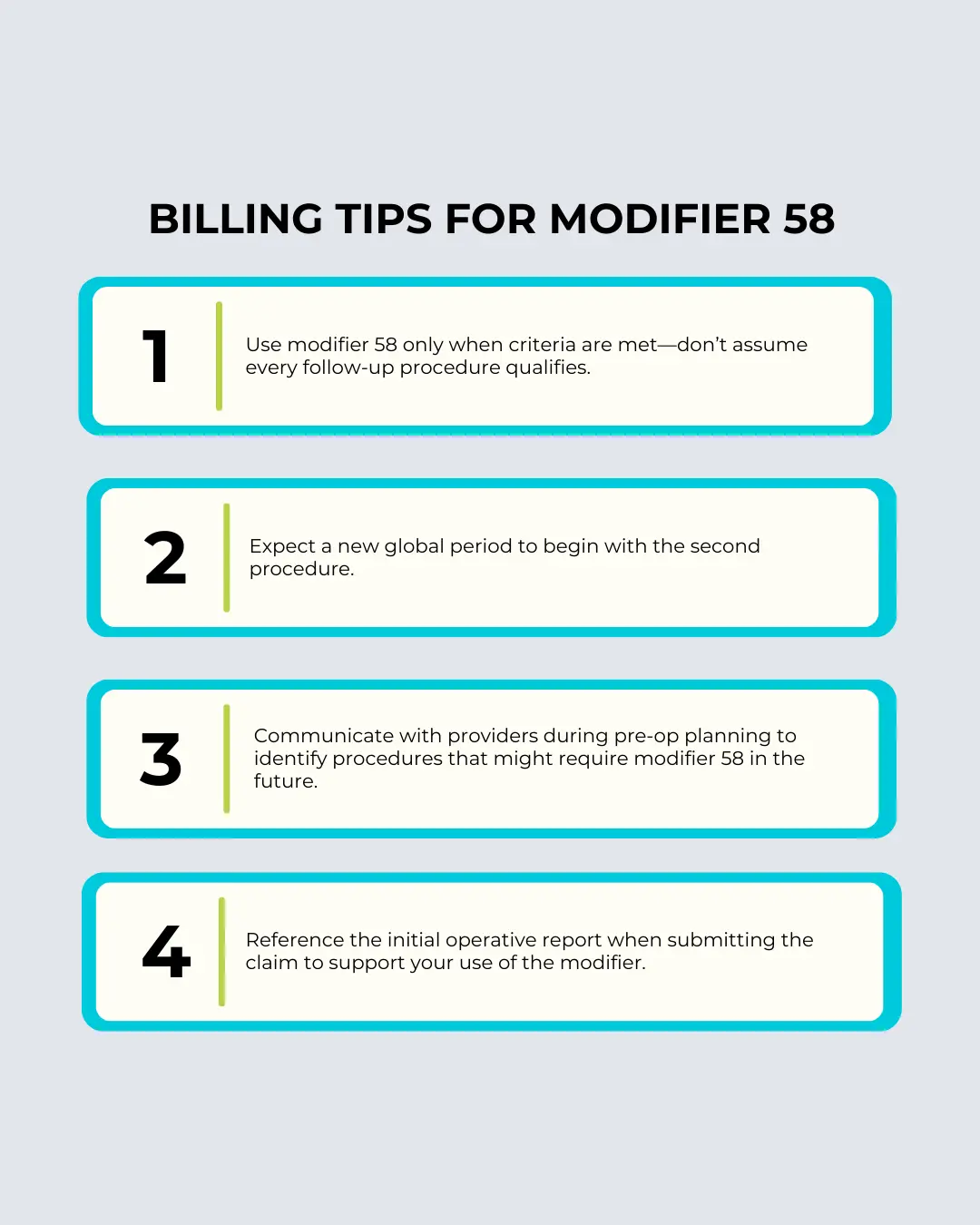
Billing Tips for Modifier 58
Modifier 58 is used to indicate a staged or planned procedure following a previous encounter. It distinguishes planned follow-up treatments from unplanned complications. Accurate documentation and proper use help ensure correct billing and prevent claim denials.
Real-World Example
Let’s say a dermatologist removes a malignant lesion and documents that additional excision will be required after reviewing pathology results. A second surgery is scheduled for wider excision two weeks later. Because this was planned at the time of the original procedure, modifier 58 is the correct choice for billing the second service.
Failing to use the right modifier in this case could lead to bundling of services or reduced reimbursement. On the other hand, using modifier 78 or modifier 79 inappropriately could trigger an audit or a denial.
Why Modifier 58 Matters in Healthcare Finance
Understanding and applying modifier 58 correctly ensures proper payment for staged or related procedures. It prevents loss of revenue and supports efficient practice management. In an industry where margins are tight and compliance risks are high, such accuracy is vital.
It also supports your medical coding team’s efforts to maintain clean claims, minimize denials, and ensure compliance with payer policies. Modifiers are more than just a two-digit code—they’re signals that affect reimbursement, audit risk, and operational efficiency.
Final Thoughts
Modifier 58 may seem like a small detail in the grand scheme of coding and billing, but it can have a major impact on your bottom line. Proper use helps ensure that your practice receives the correct reimbursement for all services rendered—especially when procedures are staged or part of a comprehensive treatment plan.
Investing time in coder education, documentation quality, and communication with providers can significantly reduce mistakes and improve your claims process. For practices and facilities looking to stay ahead of denials, audits, and revenue loss, mastering modifiers like 58 is not optional—it’s essential.
If you’re navigating complex billing requirements or struggling with denied claims, it might be time to partner with a reliable medical billing service that understands how to handle nuances like modifier 58. A knowledgeable team can ensure compliance, boost collections, and help you focus on patient care—not paperwork.
FAQS (Frequently Asked Questions)
Why is it important in billing?
It ensures correct payment for related staged procedures. Medical billing services rely on it to prevent lost revenue. It improves claim outcomes and billing accuracy.
When should you not use it?
Avoid using Modifier 58 for unplanned or unrelated procedures. Instead, consider Modifier 78 or 79. Misuse can lead to denials and compliance issues.
How does it support revenue cycle management?
Proper use of Modifier 58 improves claim accuracy and reimbursement. It supports smoother Revenue Cycle Management. This reduces denials and helps maintain financial health.
What are some common examples?
Examples include scheduled reconstructive surgery, planned hardware removal, or wider excision after biopsy. These are part of a staged treatment plan. Modifier 58 applies when the follow-up was anticipated.
Who can help with proper use?
Experienced medical coding professionals can guide correct usage. Their help minimizes denials and errors. They ensure compliance with payer rules.