Correct application of 79 modifier is crucial for distinguishing unrelated procedures performed during a postoperative period, helping providers secure appropriate reimbursement, maintain compliance, and avoid unnecessary claim denials.
When a patient receives an unrelated procedure or service during the postoperative period, understanding when and how to report it correctly can make all the difference between a clean claim and a costly denial.
What Is 79 Modifier?
The 79 modifier is used to identify a procedure or service performed during the postoperative period of another surgery, but which is completely unrelated to the original operation. It’s added to the second procedure’s CPT code to signal to payers that this treatment was medically necessary and not part of the global surgical package associated with the initial procedure.
Example in Practice:
A surgeon performs a gallbladder removal (cholecystectomy). Two weeks later, the same physician treats the same patient for a fractured arm. These are unrelated issues, so the arm procedure should be billed with 79 Modifier to clarify that it is not part of the gallbladder surgery’s global period.
Without proper coding, the payer may assume that the second procedure falls under the original global package, leading to a denial or bundled payment.
In a high-volume practice, errors like these can accumulate fast, creating inefficiencies and revenue loss. Partnering with reliable billing services medical solutions helps ensure modifiers are applied correctly and consistently.
When Should You Use 79 Modifier?
To apply the 79 modifier appropriately, the following conditions must be met:
- The procedures are unrelated: They must be for different medical conditions and involve different anatomic sites or diagnoses.
- Same physician or provider group: This rule applies when the same physician or the same group practice performs both procedures.
- Within the postoperative period: The second procedure must occur within the 10-day or 90-day global period of the original surgery.
This modifier tells insurance carriers: “Yes, the second service happened during the postoperative period, but it’s for something else entirely, and deserves independent reimbursement.”
Documentation Requirements for 79 Modifier
Proper use of 79 Modifier hinges on clear and detailed documentation. It must be obvious to payers that the services were unrelated. To avoid challenges or audits:
- Maintain separate diagnoses: The claim must show distinct ICD-10 codes for both procedures.
- Provide complete operative reports: The second procedure should be thoroughly documented to explain the necessity and timing.
- Note timeline and reasoning: Medical records should state the date and justify why the unrelated procedure was performed.
The more clearly you outline the need for the second service, the stronger your claim.
How 79 Modifier Affects Reimbursement
A properly appended modifier 79 ensures that the provider receives separate reimbursement for a distinct service performed within the global period. Without it, the second procedure may be bundled or denied.
More importantly, correct coding initiates a new global period for the second service. This can significantly impact how you manage post-op care billing and timelines for follow-up procedures.
From a broader view, mastering modifiers like 79 directly contributes to more effective healthcare revenue cycle management, reducing rework, improving collections, and minimizing payer disputes.
Common Scenarios Where Modifier 79 Applies
Here are a few real-world situations where the 79 modifier is not just helpful, but necessary:
1. Treatment on Different Body Parts
A podiatrist performs surgery on a patient’s right foot. Two weeks later, the same podiatrist treats the patient for an ingrown toenail on the left foot. These are unrelated and should be coded separately.
2. New Diagnoses During Recovery
A general surgeon performs a hernia repair. During recovery, the patient develops an unrelated skin lesion that requires excision. Since this is a new issue, 79 Modifier should be used on the skin excision.
3. Emergency Events
A cardiologist performs a stent placement. Later that month, the patient returns with a fractured wrist due to an accident. Again, these services are unrelated and should be billed with 79 Modifier.
79 Modifier vs. Modifiers 78 and 58
Understanding the differences between similar modifiers is vital:
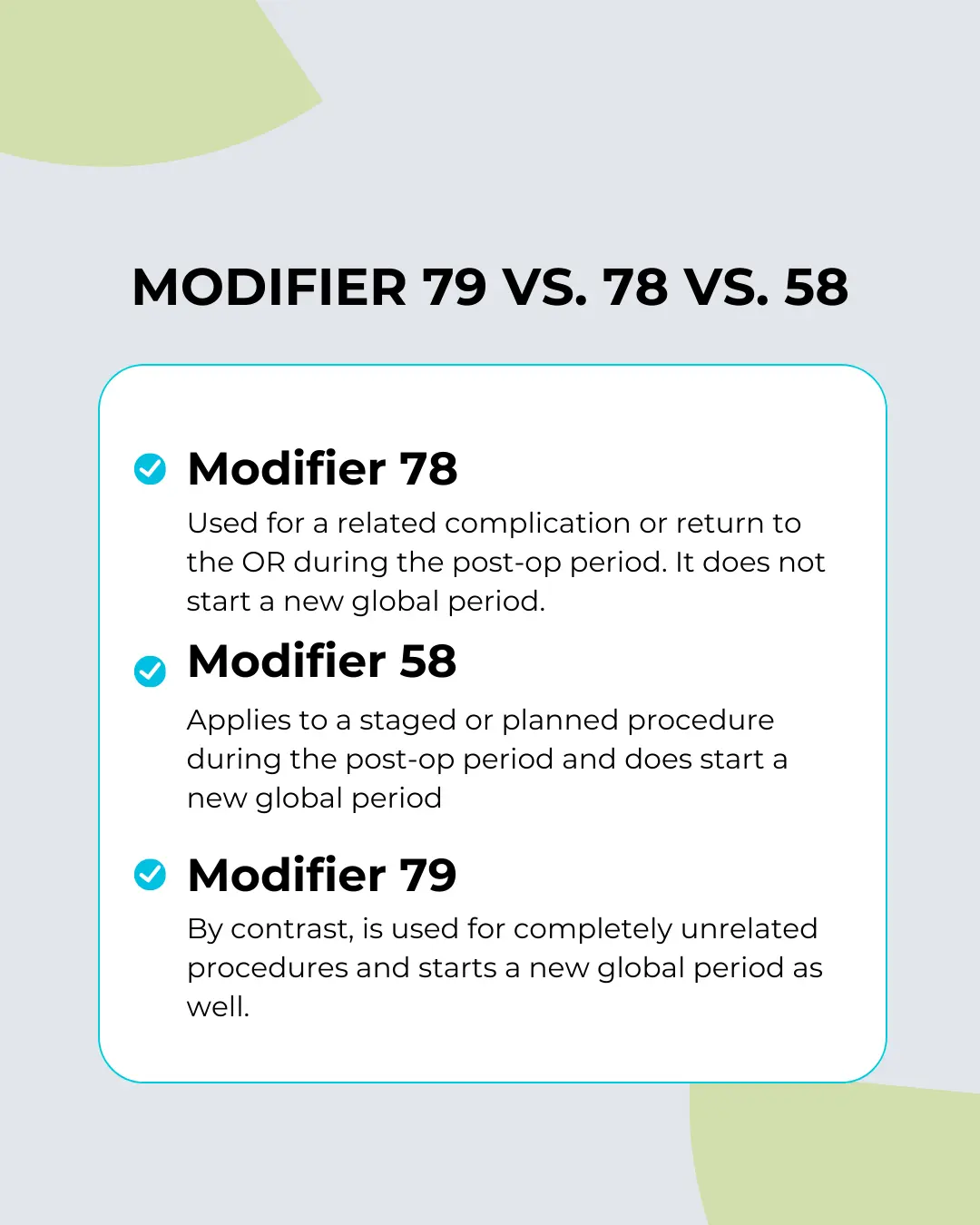
Using the wrong modifier can result in denied claims, audit triggers, and delayed payments.
How Modifier 79 Impacts Practice Efficiency
By ensuring correct usage of the 79 modifier, providers protect their revenue while maintaining compliance. It’s also an important step in maintaining efficiency within your medical billing and coding system.
Outsourced billing partners or in-house teams must:
- Recognize clinical contexts that call for 79 Modifier
- Attach accurate documentation
- Use distinct diagnosis coding to support medical necessity
An error rate as small as 5% in modifier usage can lead to hundreds of thousands of dollars in lost or delayed revenue annually, especially for high-volume specialties like surgery, orthopedics, or dermatology.
Best Practices for Using 79 Modifier
To get the most out of 79 Modifier, implement the following best practices:
- Regular Training: Educate physicians and billing staff on modifier rules and payer-specific guidelines.
- Detailed Charting: Reinforce proper charting protocols that clearly distinguish unrelated procedures.
- Audit Claims: Periodically audit claims to verify proper use of all modifiers, including 79.
- Use Technology: Leverage EHRs and billing software that flag potential modifier mismatches.
Integrating best practices into your billing workflow reduces risk, increases reimbursement, and improves compliance outcomes.
Final Thoughts
The 79 modifier may seem like just another code, but its proper use has a major impact on your practice’s financial health. It ensures that unrelated procedures during a postoperative period are recognized and reimbursed as separate and necessary services.
When used correctly, it supports accurate billing, maintains payer trust, and helps providers secure the revenue they’ve rightfully earned.
By focusing on proper modifier usage and integrating best billing practices, you’ll strengthen compliance, reduce denials, and improve outcomes across your revenue cycle.
Need help mastering 79 Modifier and other billing intricacies? Connect with experts in medical billing and coding to streamline your claims process today.