Guide physical therapy CPT codes is essential for providers aiming to ensure accurate documentation, proper reimbursement, and compliance. Whether you’re a solo practitioner or part of a larger practice, understanding the correct codes can prevent costly errors and streamline billing.
Billing services medical providers often emphasize the importance of CPT code accuracy. With numerous CPT codes used for physical therapy procedures, it’s easy to make mistakes—yet these mistakes can delay payments or trigger audits.
This guide outlines key physical therapy CPT codes, proper usage, documentation tips, and common billing challenges—all crafted to help you improve claim accuracy and revenue performance.
What Are Physical Therapy CPT Codes?
CPT (Current Procedural Terminology) codes are five-digit numeric codes used to describe medical, surgical, and diagnostic services. Physical therapy CPT codes represent the various therapeutic procedures and modalities performed by licensed therapists.
The American Medical Association (AMA) standardizes and maintains these codes, ensuring consistent service descriptions across healthcare systems.
Commonly Used Physical Therapy CPT Codes
The list below highlights the most frequently used physical therapy CPT codes:
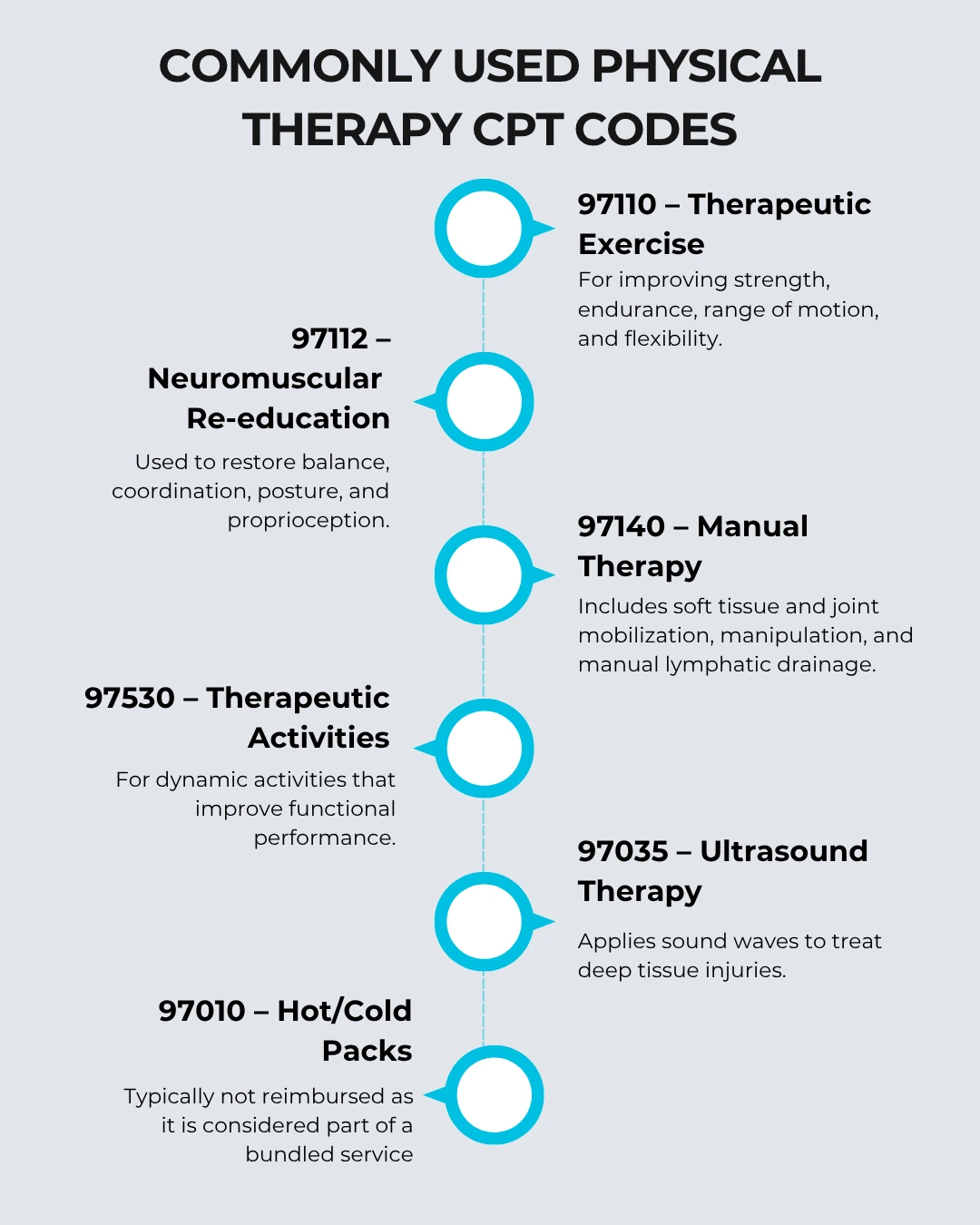
Knowing when and how to use each of these codes can maximize your billing outcomes and reduce claim denials.
Time-Based vs. Service-Based CPT Codes
Physical therapy CPT codes fall into two main categories:
- Time-Based Codes:
These require documentation of the time spent on each service. You must spend at least 8 minutes to bill one unit, based on the 8-minute rule. - Service-Based Codes:
Providers bill these once per session, regardless of time spent.
Examples:
- Time-Based: 97110, 97112, 97530
- Service-Based: 97010, 97014
Correctly distinguishing between these helps prevent overbilling and audit risks.
Documentation Best Practices for CPT Code Use
Proper documentation is the backbone of CPT code billing. Include the following in your notes:
- Type of service performed
- Duration (for time-based codes)
- Progress toward goals
- Patient response to therapy
Incomplete or vague documentation is one of the top reasons for denied or delayed payments. In the scope of healthcare revenue cycle management, every minute spent documenting accurately can lead to a stronger bottom line.
Avoiding Common Coding Mistakes
Some of the most frequent errors in using physical therapy CPT codes include:
- Undercoding or Overcoding:
Coding too little or too much can lead to underpayment or audits. - Incorrect Modifier Use:
For example, Modifier -59 indicates a distinct procedural service, and its misuse can trigger red flags. - Improper Use of Units:
Be sure to understand how many units are allowed per payer for each code.
Use billing software with integrated alerts or rely on expert coders to avoid these errors.
CPT Codes vs. ICD-10 Codes
While CPT codes describe the service, ICD-10 codes explain the medical necessity behind the service. Pairing the correct CPT code with the right ICD-10 code is essential for claim approval. For instance:
- ICD-10: M25.561 (Pain in Right Knee)
- CPT Code: 97110 (Therapeutic Exercise)
This pairing explains the reason for the therapy and supports medical necessity.
CPT Code Reimbursement Rates
Reimbursement varies based on:
- Insurance provider
- Geographic location
- Medicare fee schedules
CMS updates the Medicare Physician Fee Schedule annually. Always review the latest values or use an updated EMR system to get real-time data.
Best Practices for Maximizing Reimbursement
- Use Timely and Correct Coding:
Submit claims within the payer’s deadline using the accurate code set. - Track Denials and Trends:
Monitoring denials helps identify common issues to correct. - Invest in Training:
Keep your team trained on CPT updates to reduce errors. - Use Medical Coding Experts:
Outsourcing or hiring trained coders ensures consistent accuracy.
For long-term success, integrating expert medical coding support helps avoid lost revenue and ensures compliance.
Final Thoughts
Accurate usage of physical therapy CPT codes isn’t just about avoiding billing mistakes—it’s about creating a strong, sustainable practice. When you understand which codes to use, how to document correctly, and stay current on reimbursement policies, you’ll strengthen your revenue cycle and patient care experience.
Whether you handle billing in-house or outsource it, make sure your team is well-versed in CPT code accuracy. An efficient coding system supported by experienced professionals will always outperform a reactive, error-prone process.
Leverage your internal teams or partner with trusted industry leaders who offer specialized support in physical therapy billing and coding.
Let Precision Hub help you simplify the process and drive better financial outcomes.
FAQs (Frequently Asked Questions)
1. What are the most commonly used CPT codes in physical therapy?
Codes like 97110, 97112, 97140, and 97530 are most frequently used for therapeutic exercises and manual therapy.
2. What is the 8-minute rule in physical therapy coding?
This rule states that a time-based CPT code can be billed if the therapy service was performed for at least 8 minutes.
3. Can you bill multiple CPT codes for one session?
Yes, if multiple distinct and medically necessary services are provided, each can be billed separately with proper documentation.
4. Are hot/cold packs reimbursable in physical therapy?
Generally no. Code 97010 (hot/cold packs) is considered bundled and not separately reimbursed.
5. How do CPT codes affect my billing and reimbursement?
Incorrect coding leads to denials or underpayments. Accurate coding supports full reimbursement and compliance.