Are you confident your practice is coding common diagnoses correctly? One of the key ICD-10 codes to master is E78.5, which stands for Dyslipidemia, unspecified. This diagnosis plays a vital role in how lipid disorders are billed and reimbursed.
When you work with a professional medical billing company, you gain the expertise needed to handle such codes accurately. Correct coding not only ensures compliance but also maximizes your practice’s revenue potential.
What is Dyslipidemia and Why the E78.5 Code Matters
Dyslipidemia refers to irregular levels of fats or lipids in the blood, including cholesterol and triglycerides. Since these conditions increase cardiovascular risk, accurate diagnosis and documentation are essential.
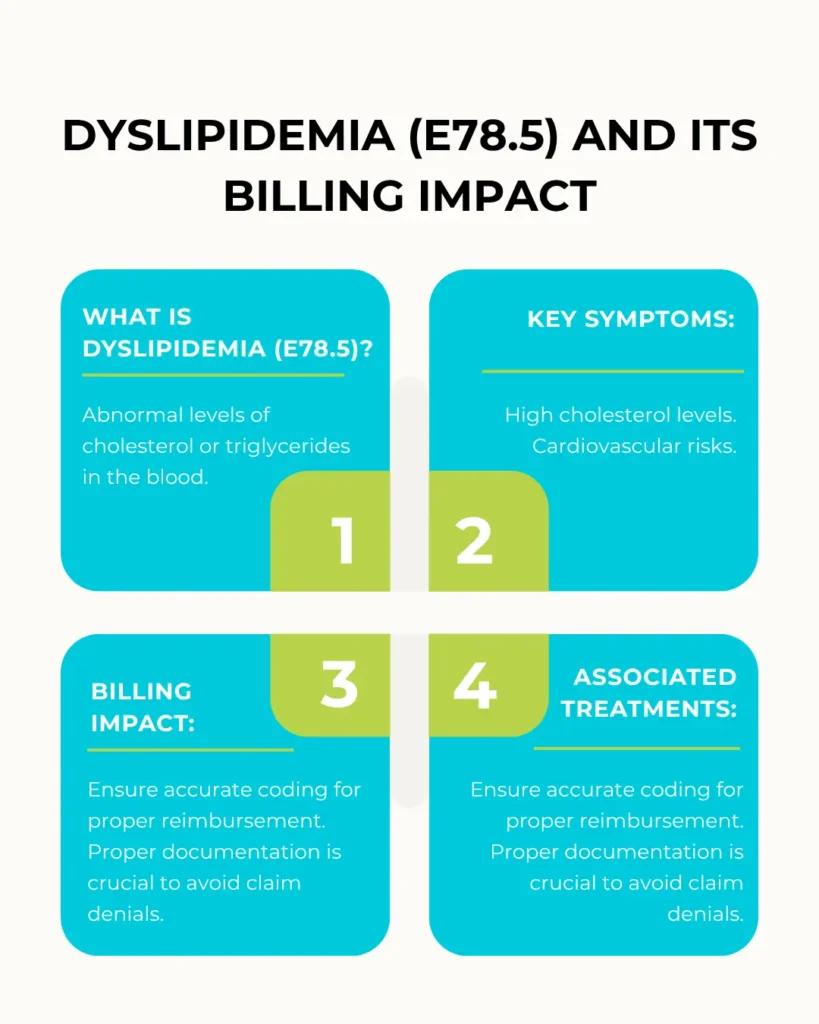
- E78.5 is used when the type of lipid disorder isn’t specified but treatment is provided.
- This code must be supported by clinical documentation to avoid claim denials.
- Proper use of E78.5 helps justify treatments, lab tests, and follow-ups.
Read more about: CAD ID 10
Optimizing Claim Processes and Patient Care
Managing claims involving E78.5 requires more than just coding. Proper coordination of clinical documentation and billing processes ensures your claims are submitted correctly and paid promptly.
When done well, this approach minimizes delays and reduces denials, keeping your practice’s revenue healthy. It also supports compliance with payer requirements, safeguarding your operations from audits and penalties.
Clear communication between providers, coders, and billers is key to maintaining this efficiency, especially for frequently coded conditions like Dyslipidemia.
Common Challenges When Coding E78.5 and How to Overcome Them
Coding the ICD-10 code E78.5 for Dyslipidemia involves several challenges that can affect billing accuracy and reimbursement. Understanding these obstacles and how to address them will help your practice improve coding quality.
Challenges
- Vague or Incomplete Documentation:
When providers use unclear terms or do not specify the lipid disorder type, coders must select the unspecified code E78.5. This lack of detail can cause claim denials or delays. - Keeping Up with Coding Updates:
Coding guidelines and payer requirements change frequently. Some insurers require additional supporting documentation like lab results or treatment plans to approve claims involving E78.5. - Communication Gaps:
Poor communication between providers and coders may lead to incorrect or incomplete coding. - Documentation and Coding Errors:
Errors during data entry or misunderstanding coding rules can result in rejected claims.
Solutions
- Enhance Provider Documentation:
Encourage clinicians to provide clear, detailed notes that specify the type of lipid disorder and related treatments. - Ongoing Coder Education:
Keep your coding team updated on the latest ICD-10 guidelines and payer policies through regular training sessions. - Regular Audits:
Perform routine audits of E78.5 coding to identify errors early and correct them before claims are submitted. - Leverage Technology:
Use electronic health records (EHR) with integrated coding assistance tools to streamline accurate documentation and code selection. - Improve Communication:
Foster collaboration between medical providers and coding staff to clarify uncertainties and ensure proper code assignment.
How Efficient E78.5 Claims
Effective Revenue Cycle Management (RCM) goes beyond submitting claims; it ensures every step supports claim approval.
- RCM teams verify that documentation aligns with E78.5 requirements.
- They manage claim submissions, rejections, and appeals efficiently.
- This process reduces delays and improves payment speed.
Moreover, RCM helps identify coding inconsistencies and educates providers on documentation improvements. Do you have a system that keeps your dyslipidemia claims on track?
Best Practices with E78.5
Accurate medical billing coding is the foundation of successful claims. For E78.5, here’s how you can stay on top:
- Ensure medical records clearly state the diagnosis and support treatment.
- Use the most specific ICD-10 codes available when possible.
- Regularly update your knowledge of coding guidelines and payer rules.
- Review claims carefully before submission to avoid errors.
- Implement audit-ready documentation practices.
By mastering these strategies, your practice can reduce claim denials and accelerate reimbursements.
Tips for Accurate Coding and Documentation
Ensuring precise coding is crucial when dealing with E78.5. Coders should verify that all supporting documentation, like lab reports, physician notes, and treatment plans, clearly support the diagnosis.
Keep your coding knowledge up to date with the latest guidelines to avoid mistakes. Errors in this area can lead to claim rejections and audit risks.
Double-check claims for accuracy and completeness before submission to maximize reimbursement and compliance.
Conclusion
Mastering the ICD-10 code E78.5 is a must for efficient medical billing related to dyslipidemia. Leveraging robust processes ensures accuracy, compliance, and faster payments. Precise medical billing coding not only safeguards your revenue but also supports better patient care documentation. Ready to optimize your billing for E78.5? It starts with understanding and applying these key practices.
FAQs
1. What does ICD-10 code E78.5 mean?
It represents unspecified dyslipidemia, indicating abnormal blood lipid levels without detailed classification.
2. Why is the correct coding of E78.5 important?
Proper coding reduces denials and ensures accurate reimbursement for related care.
3. How can a medical billing company help?
They provide expertise to optimize coding, submit claims correctly, and manage denials.
4. What role does Revenue Cycle Management play?
RCM ensures documentation supports claims and speeds up payment processing.
5. How do I avoid mistakes with E78.5 coding?
Keep documentation thorough, stay updated on guidelines, and double-check claims.