Are you looking to understand what do credentialing companies do for providers? Imagine credentialing as a healthcare professional verification stamp, allowing them to treat patients and accept insurance payments. It’s like a quality assurance verification, ensuring their qualifications are valid and they’re up to meet the standard to provide quality patient care.
This blog explains how credentialing companies help healthcare facilities and ensure the best credentialing services.
See Also: How Credentialing Specialist Fix Credentialing Issues?
Why is Credentialing Important?
Credentialing is essential for ensuring a high standard of care in the healthcare industry. It helps prevent unqualified providers from practising, protects patients’ interests, and facilitates smooth insurance reimbursement.
What Do Credentialing Companies Do for Providers?
Credentialing companies are the verification stamp for healthcare professionals. They verify a provider’s education, training, licenses, and work history to ensure they are qualified to practice medicine. This process is essential for several reasons:
1. Patient Safety
Credentialing helps protect patients by ensuring that only qualified healthcare providers treat them.
2. Insurance Reimbursement
Medical providers learn how to get credentialed with insurance companies to receive service payments.
3. Hospital Privileges
Hospitals often require providers to be credentialed before granting them privileges to practice within their facilities.
Important Tasks Performed by Credentialing Companies
Credentialing companies offer a range of services that are critical for the smooth operation of healthcare practices. These tasks include:
1. Collecting and Verifying Documents
They gather information such as medical licenses, certifications, education records, and malpractice history.
2. Assessing Qualifications
Credentialing companies evaluate whether a provider meets the specific requirements of insurance companies or healthcare organizations.
3. Communicating with Providers
They may need to contact providers to request additional documents or clarify information.
4. Updating Records
Credentialing companies maintain up-to-date records of providers’ credentials to ensure they remain qualified.
See Also: How Hospital Front Desk Staff Maximizes Billing Efficiency
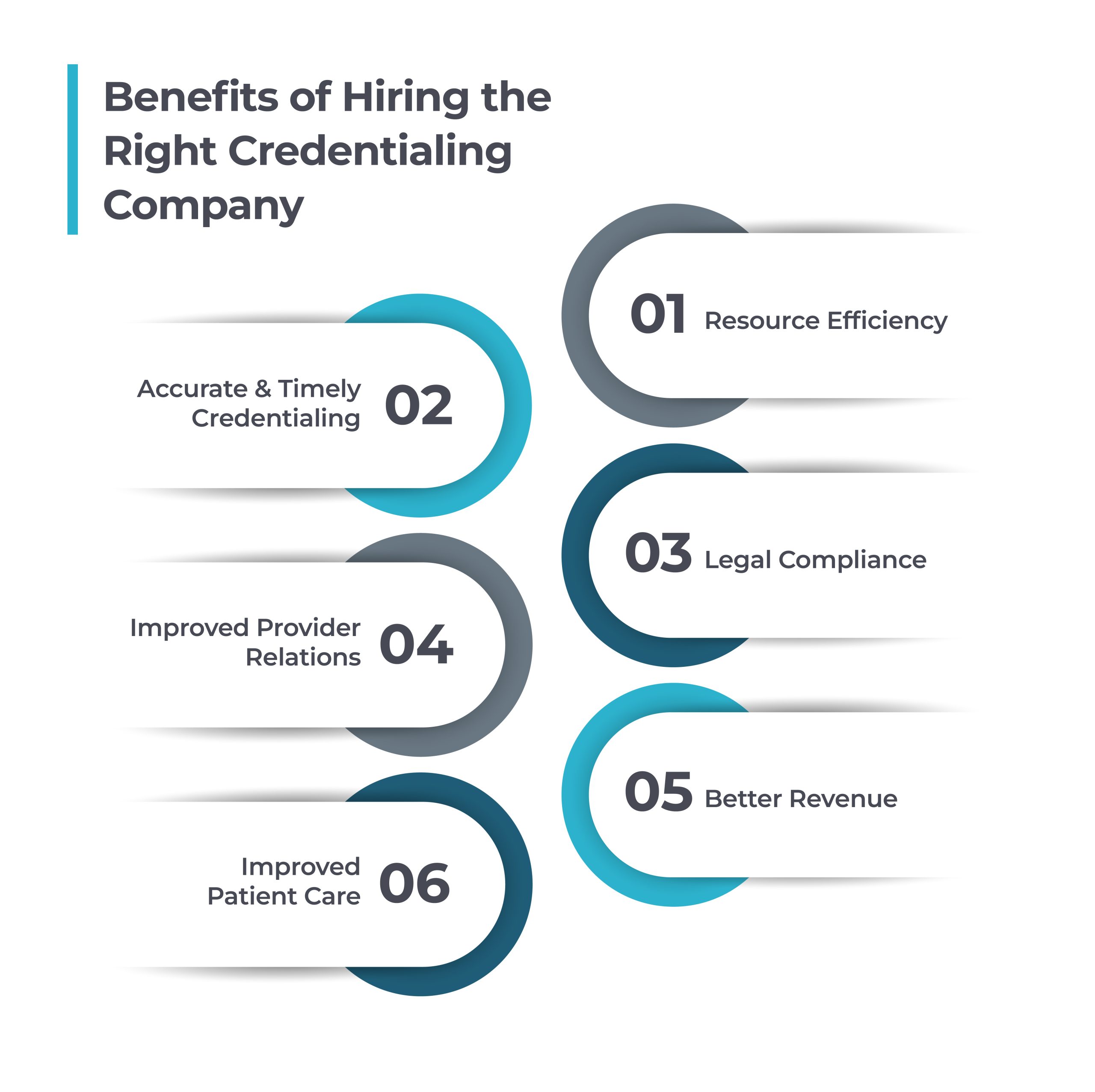
Benefits of Hiring the Credentialing Company
Credentialing is a crucial process that verifies the qualifications and experience of healthcare professionals. Choose the right credential solutions can offer significant benefits to your healthcare organization. Here are some key advantages.
1. Resource Efficiency
By entrusting credentialing to specialized companies, healthcare organizations can significantly streamline processes, efficiently manage complex and time-consuming tasks, and improve overall healthcare outcomes.
2. Accurate & Timely Credentialing
Credentialing companies possess in-depth knowledge of the latest regulations and requirements, ensuring accurate and timely completion of the credentialing process and saving healthcare organizations valuable time and resources.
3. Legal compliance
By partnering with a credentialing company, healthcare organizations can ensure that their providers meet all regulatory standards, thereby mitigating the risk of penalties and legal complications.
4. Improved Provider Relations
Credentialing companies offer valuable support and guidance to healthcare providers throughout the insurance credentialing process, handling these time-consuming responsibilities to improve provider satisfaction and efficiency.
5. Better Revenue
Accurate credentialing accelerates payer reimbursement and expands patient access. Healthcare organizations can widen their reach and attract a broader patient base, leading to increased revenue and improved patient care.
6. Improved Patient Care
Credentialing ensures that only qualified healthcare providers are entrusted with patient care. This builds trust, and they know they are getting the best services according to credentialing standards.
Also See: Addressing Medical Credentialing Issues & Its Solutions
Conclusion
Credentialing is a vital verification process in the healthcare system. It ensures patients receive care from qualified providers and helps healthcare organizations maintain their reputation and financial stability.
In today’s competitive healthcare industry, understanding what credentialing companies do for providers helps in hiring the right support services. Credentialing is an essential process that ensures quality care and can simplify operations for patients and medical providers.
Precision Hub: Your Trusted Partner
By understanding the importance of provider credentialing in healthcare facilities, you can choose Precision Hub’s complete credentialing services customized to your practice needs. Our services ensure your providers are qualified and recognized by payers, leading to improved reimbursement and patient access.
Ready to hire the best medical credentialing company for your practice?
Contact Precision Hub today to learn how our credentialing services can help verify your details and expedite claim processing.